1
UNIVERSIDADE FEDERAL DE PELOTAS
Programa de Pós-Graduação em Biotecnologia
Dissertação
VACINA TERAPÊUTICA: AVALIAÇÃO DE Mycobacterium bovis BCG
RECOMBINANTE PARA IMUNOTERAPIA DE CÂNCER SUPERFICIAL DE
BEXIGA
KARINE RECH BEGNINI
Pelotas, 2012
2
KARINE RECH BEGNINI
VACINA TERAPÊUTICA: AVALIAÇÃO DE Mycobacterium bovis
BCG RECOMBINANTE PARA IMUNOTERAPIA DE CÂNCER
SUPERFICIAL DE BEXIGA
Dissertação apresentada ao Programa de
Pós-Graduação em Biotecnologia da
Universidade Federal de Pelotas, como
requisito parcial à obtenção do título de
Mestre
em
Ciências
(área
do
conhecimento: Biotecnologia).
Orientadora: Prof.ª Fabiana Kömmling Seixas, Dra.
Comissão de Orientação: Prof. João Carlos Deschamps, PhD.
Prof. Odir Antônio Dellagostin, Dr.
Prof. Tiago Collares, Dr.
Pelotas, 2012
3
Dados de catalogação na fonte:
Ubirajara Buddin Cruz – CRB 10/901
Biblioteca de Ciência & Tecnologia - UFPel
B417v
Begnini, Karine Rech
Vacina terapêutica: avaliação de Mycobacterium bovis
bcg recombinante para imunoterapia de câncer superficial de
bexiga / Karine Rech Begnini. – 60f. : gráf. – Dissertação
(Mestrado). Programa de Pós-Graduação em Biotecnologia.
Universidade Federal de Pelotas. Centro de Desenvolvimento
Tecnológico, 2012. – Orientador Fabiana Kömmling Seixas ;
co-orientador João Carlos Deschamps, Odir Antônio
Dellagostin, Tiago Collares.
1.Biotecnologia.
2.Bacillus
Calmette-Guérin.
3.BCG
recombinante. 4.Câncer superficial de bexiga. 5.Atividade
antitumoral. 6.Imunoterapia. I.Seixas, Fabiana Kömmling.
II.Deschamps, João Carlos. III.Dellagostin, Odir Antônio.
IV.Collares, Tiago. V.Título.
CDD: 615.372
4
Banca examinadora:
Prof.ª Fabiana Kömmling Seixas, Universidade Federal de Pelotas
Prof. Alan McBride, Universidade Federal de Pelotas
Prof.ª Sandra Beatriz Chaves Tarquínio, Universidade Federal de Pelotas
Prof.ª Sibele Borsuk, Universidade Federal de Pelotas
5
AGRADECIMENTOS
À Universidade Federal de Pelotas pela oportunidade de realizar um curso de
Pós-Graduação de qualidade
À Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES)
pela concessão da bolsa de estudos.
A minha orientadora, Dra. Fabiana K. Seixas, pela confiança e experiência,
pelo comprometimento, carinho e incentivo dispensados na realização deste
trabalho, o qual contribuiu para meu amadurecimento e formação profissional.
Aos meus amados pais Henrique e Eliana, pela educação que me foi dada,
pelo apoio, por acreditarem em meus sonhos e tornar sua realização possível. Eles
são os grandes responsáveis pela minha formação pessoal.
Aos meus irmãos Guilherme e Eduardo, companheiros de todas as horas,
agradeço pelo carinho e apoio, mesmo que muitas vezes à distância.
Ao meu namorado e amigo Guilherme Reissig, pelo carinho nos momentos de
dúvida, pelo amor e companheirismo nos momentos de conquistas e perdas, e pela
compreensão durante minhas ausências.
A toda a grande família GPO, pelos sempre divertidos momentos vividos no
laboratório e nas rodas de café.
Às queridas companheiras e amigas de cultivo celular Virgínia, Eduarda e
Priscila pelo companheirismo durante as muitas idas extras ao campus, pela ajuda
na execução dos experimentos, pela divisão dos problemas e por tornar os dias de
trabalho mais divertidos.
Às colegas e amigas Carolize Rizzi e Karen Leal, por toda a paciência e
ensinamentos.
Aos colegas, estagiários e amigos do Centro de Biotecnologia, pela amizade
e convívio agradável.
A todos que de uma forma ou outra auxiliaram no desenvolvimento desta
dissertação, fazendo parte de mais uma etapa de minha vida.
Muito obrigada!
6
RESUMO
BEGNINI, Karine Rech. Vacina terapêutica: avaliação de Mycobacterium bovis BCG
recombinante para imunoterapia de câncer superficial de bexiga. 2012. 60fs.
Dissertação (Mestrado) - Programa de Pós-Graduação em Biotecnologia. Universidade
Federal de Pelotas, Pelotas.
O Bacilo Calmette-Guérin (BCG) constitui uma das grandes histórias de sucesso da
imunoterapia como tratamento para carcinoma superficial da bexiga. Porém, a alta
incidência de efeitos colaterais locais e a ocorrência de tumores resistentes ao tratamento
têm impulsionado estudos visando melhorias da vacina terapêutica. Neste trabalho,
propusemos que uma cepa auxotrófica de BCG superexpressando o antígeno Ag85B
(BCG ΔleuD/Ag85B), é capaz de aumentar a citotoxicidade na linhagem celular humana de
carcinoma superficial de bexiga (5637). A cepa de BCG recombinante foi gerada através da
incorporação da sequencia do antígeno Ag85B em um plasmídeo de expressão
micobacteriano na cepa de BCG ΔleuD. O efeito inibitório do BCGΔleuD/Ag85B em células
5637 foi determinada através das técnicas colorimétricas MTT e LIVE/DEAD, além de
observação morfológica. Os perfis de expressão gênica para genes apoptóticos, genes
relacionados ao ciclo celular e genes de estresse oxidativo foram avaliados por qRT-PCR.
Os níveis protéicos de bax, bcl-2 e p53 foram avaliados por western blot. O BCG
ΔleuD/Ag85B revelou citotoxicidade superior às cepas utilizadas como controle neste
estudo. Os resultados obtidos demonstram níveis superiores de expressão de genes próapoptóticos e de genes relacionados com o ciclo celular após tratamento com
BCG ΔleuD/Ag85B. Níveis inferiores de mRNA de genes antiapoptóticos foram detectados
após o mesmo tratamento. Ainda, o tratamento com BCG ΔleuD/Ag85B também elevou os
níveis de mRNA de enzimas antioxidantes em linhagem de células de câncer superficial de
bexiga. As proteínas Bax e p53 mostraram-se elevadas após tratamento com
BCG ΔleuD/Ag85B. Em conclusão, estes resultados sugerem que a cepa de BCG
superexpressando Ag85B é capaz de aumentar a citotoxicidade sobre as células de câncer
superficial de bexiga in vitro. Este modelo terapêutico usando BCG recombinante possui
potencial para uma futura aplicação clínica em tratamento de câncer de bexiga.
Palavras chave: Bacillus Calmette-Guérin. BCG recombinante. Câncer superficial de
bexiga. Atividade antitumoral.
7
ABSTRACT
BEGNINI, Karine Rech. Vacina terapêutica: avaliação de Mycobacterium bovis BCG
recombinante para imunoterapia de câncer superficial de bexiga. 2012. 60fs.
Dissertação (Mestrado) - Programa de Pós-Graduação em Biotecnologia. Universidade
Federal de Pelotas, Pelotas.
Bacillus Calmette-Guerin (BCG) is one of the great success stories of immunotherapy as a
treatment for superficial urothelial carcinoma of the bladder. The high incidence of local side
effects and presence of non-responder diseases has led to efforts to improve the therapeutic
vaccine. Hence, we proposed that an auxotrophic recombinant BCG strain overexpressing
Ag85B (BCG ∆leuD/Ag85B), could enhance cytotoxicity to the human bladder carcinoma cell
line (5637). This rBCG was generated by incorporating an expression plasmid encoding the
mycobacterial antigen Ag85B into the BCG ∆leuD strain. The inhibitory effect of BCG
∆leuD/Ag85B in 5637 cells was determined by the MTT method, morphology observation
and the LIVE/DEAD assay. Gene expression profiles for apoptotic genes, cell cycle-related
genes and oxidative stress-related genes were investigated by qRT-PCR. Bax, bcl-2 and p53
induction by BCG ∆leuD/Ag85B treatment were evaluated by Western blotting. BCG
∆leuD/Ag85B revealed a superior cytotoxicity effect than the strains used as controls in this
study. The results demonstrated that the expression level of pro-apoptotic and cell cyclerelated genes increased after BCG ∆leuD/Ag85B treatment, whereas mRNA levels of
antiapoptotic genes decreased. Interestingly, BCG ∆leuD/Ag85B also increased the mRNA
level of antioxidant enzymes in bladder cancer cell line. Bax and p53 protein levels were
increased by BCG ∆leuD/Ag85B treatment. In conclusion, these results suggested that BCG
∆leuD/Ag85B enhanced cytotoxicity on superficial bladder cancer cells in vitro. The
therapeutic model using rBCG may have potential for future clinical application in the
treatment of bladder cancer.
Keywords: Bacillus Calmette-Guérin. Recombinant BCG. Superficial bladder cancer.
Antitumor activity.
8
LISTA DE FIGURAS
Figura 1*
Mecanismo de ação do bacilo de Calmette-Guérin frente a células de
carcinoma de bexiga.
17
Figura 1A
Western blot demonstrando a expressão de Ag85B em BCG Pasteur
∆leuD.
42
Figura 1B
MTT mostrando o efeito citotóxico de cepas de BCG em células
5637 após 48 h de co-cultivo.
42
Figura 2
Ensaio colorimétrico LIVE/DEAD de células tratadas e não tratadas
com cepas de BCG por 48 horas.
43
Figura 3
Efeito de cepas de BCG sobre os níveis de mRNA de genes
apoptóticos.
44
Figura 4
Efeito de cepas de BCG sobre os níveis de mRNA de caspases.
45
Figura 5
Efeito de cepas de BCG sobre os níveis de mRNA de enzimas
antioxidantes.
.
Efeito de cepas de BCG sobre os níveis de mRNA de genes
relacionados ao ciclo celular.
46
Figura 6
47
9
LISTA DE TABELAS
Tabela 1
Primers utilizados neste estudo.
41
10
LISTA DE ABREVIATURAS E SIGLAS
BCG – Bacillus Calmette-Guérin
wtBCG – BCG do tipo selvage (wild type)
qRT-PCR – PCR em tempo real
TNF – Tumor necrosis factor
IL-1 – Interleucina-1
IL-2 – Interleucina-2
IL-6 – Interleucina-6
IL-8 – Interleucina-8
IL-10 – Interleucina-10
IL-12 – Interleucina-12
TNF-α – Tumor necrosis factor α
IFN-γ – Interferon γ
11
SUMÁRIO
1. Introdução.......................................................................................
10
1.1 Carcinomas de bexiga...........................................................
10
1.2 Imunoterapia...........................................................................
11
1.3 Mycobacterium bovis BCG.....................................................
13
1.4 M. bovis BCG e câncer...........................................................
13
1.5 Mecanismos de ação..............................................................
14
1.6 BCG recombinante.................................................................
16
1.7 Antígeno Ag85B...................................................................... 18
2. Objetivos.........................................................................................
19
2.1 Geral.......................................................................................
19
2.2 Específicos.............................................................................. 19
3. Artigo...............................................................................................
20
3.1 Abstract................................................................................... 22
3.2 Introduction.............................................................................
23
3.3 Material and Methods.............................................................
24
3.4 Results....................................................................................
28
3.5 Discussion............................................................................... 31
3.6 References.............................................................................. 34
4. Conclusões.....................................................................................
48
5. Referências.....................................................................................
49
12
1. INTRODUÇÃO
1.1 Carcinomas de bexiga
O câncer de bexiga é o quarto tipo de tumor mais comum em homens e o
décimo primeiro mais comuns em mulheres (SIEGEL et al., 2011). Possui forte
impacto
econômico no
sistema
de
saúde
mundial
e
é
responsável
por
aproximadamente 5% de todas as mortes por câncer (SIMONS et al., 2007). No
Brasil, a incidência e mortalidade por câncer de bexiga são menores do que aquelas
relatadas em países desenvolvidos, embora haja uma tendência de aumento no
número de casos nos últimos anos. Segundo estatísticas nacionais, estimam-se
aproximadamente 8.900 novos de câncer na bexiga para o ano de 2012 (INCA,
2012).
Neoplasias da bexiga são 2,5 vezes mais freqüentes em homens que em
mulheres (PASHOS et al., 2002) e possuem como principal fator de risco o
tabagismo (INCA, 2012). Além disso, exposição ocupacional a aminas aromáticas,
infecção por Schistosoma hematobium, infecções urinárias recorrentes e consumo
excessivo de café também parecem ter associação positiva para esse tipo de câncer
(ZEEGERS et al., 2000; INCA, 2012). Genética e molecularmente falando, esta
neoplasia apresenta associações com inibição do gene supressor de tumor p53,
deleções no cromossomo 9 e ativação de oncogenes, como c-erb-B2, HER-2/neu e
H-ras (JUNG; MESSING, 2000).
Cerca de 80% dos tumores vesicais são do tipo carcinoma superficial de
bexiga (carcinoma in situ). Este tipo de tumor se caracteriza por possuir altas taxas
de recorrência (69-80%) e predisposição para progredir como tumor músculoinvasivo (33-48%) (SYLVESTER et al., 2005). Carcinomas superficiais de bexiga
geralmente se originem de uma única hiperplasia urotelial nodular e se tratados
precocemente por ressecção cirúrgica e imunoterapia intravesical a taxa de
sobrevida chega a 90% em cinco anos (WU, 2005). Tumores invasivos ou músculo-
13
invasivo da bexiga constituem a segunda forma de neoplasia urotelial e acometem
aproximadamente 20% dos pacientes vesicais. Caracterizado por sua alta
agressividade, este tipo de tumor se origina através de mecanismos de novo ou
através de lesões planas de alto grau oriundas dos carcinomas in situ. O tratamento
para tumores invasivos constitui de cistectomia radical e quimioterapias sistêmicas,
no entanto, as taxas de sobrevida são bastante limitadas, chegando a apenas 6%
em dois anos para pacientes metastáticos (WU, 2005).
Um dos grandes desafios da terapêutica para carcinomas de bexiga é a
identificação de pacientes com carcinomas in situ que irão apresentar recorrência ou
progressão invasiva (SCHENK-BRAAT; BANGMA, 2005). O tratamento padrão para
câncer superficial de bexiga baseia-se em cirurgia endoscópica associada a terapia
intravesical complementar, que tem como objetivo principal promover efeito
antineoplásico através da estimulação do sistema imunológico e da secreção de
citocinas (THALMANN et al., 2000). Instilações vesicais de Mycobacterium bovis
BCG representam o tratamento vesical de escolha para este tipo de tumor, visando
a eliminação residual da doença e reduzindo o risco de possíveis recidivas e
progressões musculares (GONTERO et al., 2010). Aprovada em 1990 pela FDA, a
imunoterapia com instilação intravesical de BCG é considerada o tratamento padrão
ouro para carcinomas in situ (AMIRKHAH et al., 2009).
1.2 Imunoterapia
A imunoterapia é uma estratégia alternativa e potencialmente eficaz para
tratamento de câncer, baseada na especificidade do sistema imunológico e na sua
limitada toxicidade (ALDRICH et al., 2010). O conceito de imunoterapia geralmente
envolve a geração de uma resposta ativa contra antígenos associados a tumores
(TAAs) (SHENG; HUANG, 2011). Dessa forma, constitui um tratamento que
promove estimulação do sistema imune por meio do uso de substâncias
modificadoras da resposta biológica (ALDRICH et al., 2010).
O sistema imunológico é capaz de reconhecer e extinguir lesões précancerosas e cancerosas (SHENG; HUANG, 2011). Esse reconhecimento é obtido
principalmente através de vacinação com peptídeos antigênicos ou através de
células dendríticas ativadas. A administração de moduladores imunes, como
citocinas, também pode impulsionar a imunidade antitumoral existente e levar
células efetoras da vigilância imunológica aos locais de crescimento do tumor
14
(DRANOFF, 2004). Quando comparada com quimio ou radioterapia, a utilização de
tratamento
imunoterapêutico
apresenta
duas
vantagens
potenciais:
(a)
especificidade para com a célula-alvo, reduzindo assim os efeitos adversos nos
tecidos sadios; e (b) menor interferência em outras terapias, tornando-se um
tratamento adjuvante adequado às terapias convencionais (SHENG; HUANG, 2011).
Em tumores de bexiga, a imunoterapia utilizando M. bovis BCG é considerada
tratamento de escolha para carcinomas in situ (GONTERO et al., 2010). Além disso,
é o único agente conhecido capaz de reduzir as taxas de recorrência e de
progressão muscular da doença, obtidas através da ativação do sistema imune
(SYLVESTER et al., 2002).
Vacinas anticâncer constituem foco importante na imunoterapia. Em termos
de câncer, a vacinação se baseia em duas estratégias principais: a utilização de
vacinas profiláticas, que imunizam o paciente contra infecções de vírus oncogênicos,
como HPV, ou que previnem o desenvolvimento de tumores em indivíduos
pertencentes a grupos de risco; ou a utilização de vacinas terapêuticas, focadas no
combate a doenças já estabelecidas (MADAN et al., 2010). A produção de vacinas
profiláticas para câncer tem se mostrado ineficiente principalmente devido ao fato de
que antígenos tumorais são normalmente variações de proteínas próprias do
organismo, que podem acarretar em complicações autoimunes (AMOS et al., 2011).
Durante décadas a vacinação terapêutica não foi considerada uma terapia padrão
para câncer. No entanto, a aprovação no ano de 2010, pela FDA, de uma vacina de
células dendríticas (DC) para tratamento de câncer de próstata ressaltou o sucesso
da utilização do sistema imune no combate à doença e tem incentivado o
desenvolvimento de pesquisa visando a utilização combinada destes componentes
imunológicos com a quimioterapia padrão (ANASSI; NDEFO, 2011).
É
importante
salientar
que
as
condições
observadas
durante
o
desenvolvimento de uma resposta imune antitumoral diferem das circunstâncias
prevalentes durante uma infecção por patógeno (GILBOA, 2004). Durante a
replicação de um patógeno, a ativação de células T reativas é controlada, de
maneira a causar pouco ou nenhum dano fisiológico; o que não ocorre no caso da
imunoterapia contra tumores. A utilização de antígenos não-específicos ao tumor e
repetições sucessivas de doses vacinais podem ativar células T autorreativas e
gerar poderosas respostas autoimunes (AMOS et al., 2011). Dessa forma, a escolha
do antígeno pode constituir um fator chave no controle do desenvolvimento da
15
imunidade e escolhas ideais priorizariam antígenos que são normalmente expressos
em sítios imunoprivilegiados ou ainda aqueles que são específicos ao tumor
(SCHREIBER et al., 2011).
1.3 Mycobacterium bovis BCG
O Bacillus Calmette-Guérin (BCG) é uma cepa viva atenuada da bactéria
Mycobacterium bovis, utilizada principalmente como vacina para formas graves de
tuberculose (BENEVOLO-DE-ANDRADE et al., 2005). Desenvolvido em 1921 por
Albert Calmette e Camille Guérin, o BCG sofreu sucessivos subcultivos, o que
resultou na atenuação da cepa original. A utilização dessa vacina em humanos, bem
como sua produção em larga escala, ocorreu em 1924, no Instituto Pasteur de Lille,
na França (BENEVOLO-DE-ANDRADE et al., 2005).
Desde 1924, subcepas da bactéria M. bovis BCG foram encaminhadas a
diferentes países, originando variantes que apresentam diferenças bioquímicas,
moleculares, morfológicas e imunológicas (BEHR; SMALL, 1999). Cada uma dessas
cepas é nomeada pelo país ou laboratório onde foi propagada, sendo conhecidas
hoje mais de 50 subcepas de BCG (LAGRANDERIE et al., 1996). No entanto,
somente seis delas estão atualmente em uso como vacina para tuberculose: BCG
Connaught, BCG Glaxo, BCG Moreau, BCG Pasteur, BCG Tokyo e BCG Danish
(MINNIKIN et al., 1984). A cepa de BCG utilizada no Brasil foi cultivada pela primeira
vez em 1925, pelo médico uruguaio Julio Moreau, sendo nomeada como BCG
Moreau Rio de Janeiro (BENEVOLO-DE-ANDRADE et al., 2005). Apesar das
variações que ocorrem entre as diferentes cepas, todas mantiveram alguma eficácia
tanto para vacinação como para imunoterapia (HERR; MORALES, 2008).
1.4 M. bovis BCG e câncer
Observações a respeito dos efeitos antitumorais do BCG vêm sendo descritas
há bastante tempo. A existência de uma relação entre a tuberculose e o câncer foi
primeiramente proposta por Pearl et al (1929). Após uma série de autópsias, o autor
notou menor incidência de câncer e maior sobrevida em pacientes que
apresentavam tuberculose ativa ou prévia, sugerindo a existência de um
antagonismo entre estas entidades (PEARL et al, 1929). No entanto, o uso do BCG
em oncologia foi somente proposto de forma concreta em 1959 após estudos que
demonstraram que camundongos infectados com BCG apresentavam resistência a
16
tumores transplantáveis, através do aumento da reatividade imunológica (OLD et al.,
1959).
Os efeitos antitumorais da administração de BCG em tumores de bexiga foi
descrita pela primeira vez em 1976 por Morales et al. A inibição do crescimento
tumoral após instilação de BCG foi observada e esse efeito foi atribuído
primeiramente a uma reação imunológica de hipersensibilidade do tipo tardio
(MORALES et al., 1976). Os mecanismos de atuação da bactéria frente a neoplasias
passou a ser melhor compreendido em 1971 com a publicação de um estudo
demonstrando uma redução da implantação e do crescimento tumoral, quando uma
nova aplicação de células neoplásicas era realizada subseqüente à inoculação de
BCG (ZBAR; TANAKA, 1971). Desde então, diversos estudos confirmaram que a
aplicação de BCG intravesical é capaz de eliminar células remanescentes, retardar a
progressão da doença e melhorar a sobrevida dos pacientes com câncer superficial
de bexiga (COE; FELDMAN, 1966; MATHE et al., 1969; LAMM et al., 1980). Em
1990, a FDA aprovou o uso clínico de BCG no tratamento de pacientes oncológicos
(AMIRKHAH et al., 2009).
1.5 Mecanismos de ação
Um sistema imune eficiente constitui pré-requisito para o sucesso de uma
imunoterapia utilizando BCG. Embora não esteja completamente elucidado,
acredita-se que o mecanismo de ação da terapia intravesical com BCG para tumores
esteja relacionado com uma estimulação local e inespecífica do sistema imune pela
bactéria (BOHLE; BRANDAU, 2003; LIU et al., 2009). Pacientes sob tratamento para
carcinoma in situ apresentam presença elevada de citocinas na urina, principalmente
IL-1, IL-2, IL-6, IL-8, IL-12, TNF-α, INF-γ e GM-CSF. Este perfil de citocinas próinflamatórias, especialmente IL-2, TNF-α e INF-γ, constitui um padrão de secreção
de resposta imune do tipo Th1 (ANDRADE et al., 2010). Em camundongos, tem se
observado que a presença de INF-γ e IL-12 se faz necessária para o controle
imunoterápico de câncer de bexiga, sendo sugerido que terapias efetivas para este
tipo de tumor requerem ativação de resposta imune Th1 (ANDRADE et al., 2010).
Primeiramente, o BCG induz um afluxo maciço de células inflamatórias na
mucosa e no lúmen da bexiga, levando a uma resposta imune contra células
tumorais (BOHLE; BRANDAU, 2003). Quando é feita a instilação intravesical de
BCG, uma parte dos bacilos injetados na bexiga adere à parede vesical e se liga às
17
células uroteliais, através de fibronectinas, sendo em seguida internalizado por
essas células (KRESOWIK; GRIFFITH, 2009). Estudos in vitro têm demonstrado
que, embora a ativação do sistema imune seja uma etapa crucial para o sucesso da
terapia com BCG, algumas cepas de BCG são capazes de atuar diretamente
sobre as células tumorais após a internalização, promovendo uma inibição da
proliferação por apoptose (ZHENG et al., 2011). Ademais, internalização da bactéria
leva
a
produção
(KRESOWIK;
de
citocinas,
GRIFFITH,
2009).
desencadeando
Células
um
processo
inflamatórias,
como
inflamatório
leucócitos
polimorfonucleares e neutrófilos, se infiltram no local e desencadeiam a liberação de
grandes quantidades de citocinas, que levam ao recrutamento de outros tipos de
células imunes. A resposta celular primária é constituída principalmente de
neutrófilos e macrófagos, porém num segundo momento, células T CD4+ são
predominantes no local (BOHLE; BRANDAU, 2003).
Além disso, a citocina TNF-related apoptosis-inducing ligand (TRAIL) parece
ser um contribuinte importante para o efeito antineoplásico da imunoterapia com
BCG (LUDWIG et al., 2004). TRAIL é um membro da família TNF que induz
apoptose em células neoplásicas, mas não em células e tecidos saudáveis
(LUDWIG et al., 2004). A expressão de TRAIL pode ser induzida por muitas
populações de células inflamatórias, após estímulo com citocinas, especialmente
com interferons do tipo I e II (KRESOWIK; GRIFFITH, 2009). Estudos recentes tem
demonstrado que pacientes que respondem corretamente a instilação intravesical de
BCG possuem quantidade maior de TRAIL na urina do que aqueles que não
respondem ao tratamento e que, além disso, naqueles em que o tratamento é eficaz,
a quantidade de TRAIL na urina é crescente após cada aplicação subseqüente de
BCG (LUDWIG et al., 2004).
Neutrófilos são as principais células responsáveis pela secreção da citocina
TRAIL. Análises da urina de pacientes com infecções diversas do trato urinário
mostrou baixos níveis dessa citocina nas amostras, quando comparado com
pacientes que tiveram estimulação com BCG, sugerindo que a resposta TRAIL é
específica para a micobactéria (KRESOWIK; GRIFFITH, 2009). Além disso, a
estimulação de neutrófilos do sangue periférico com diversas espécies bacterianas
mostrou que apenas o BCG é capaz de estimular a liberação de TRAIL
(KRESOWIK; GRIFFITH, 2009). Uma representação visual do mecanismo de ação
proposto para o BCG encontra-se ilustrado na Figura 1.
18
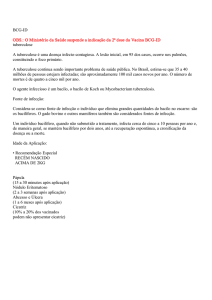
Figura 1: Mecanismo de ação do bacilo de Calmette-Guérin frente a células de
carcinoma de bexiga. (A) A infecção de células uroteliais por BCG leva a liberação
de citocinas, como IL-8. (B) Neutrófilos constituem as células iniciais de resposta ao
BCG; a presença da micobactéria estimula a liberação de TRAIL e de fatores
quimiotáticos por estas células. (C) Células inflamatórias efetoras, como células T e
macrófagos, respondem aos sinais quimiotáticos secretados pelos neutrófilos. (D) A
presença de células citotóxicas e da citocina TRAIL induz à apoptose tumoral.
Adaptado de: Kresowik & Griffith, 2009.
BCG: Bacille Calmette–Guerin; TRAIL: TNF-related apoptosis-inducing ligand.
1.6 BCG recombinante
O sucesso do BCG como agente imunoterápico vem promovendo o
desenvolvimento de pesquisas que buscam maneiras de manter ou melhorar sua
eficácia terapêutica, porém reduzindo o perfil de efeitos colaterais (ANDRADE et al.,
2010). Embora seja considerada a terapia intravesical mais eficaz no tratamento de
tumores superficiais de bexiga, alguns problemas podem ocorrer levando ao
surgimento de tumores intolerantes, resistentes ou recorrentes (GONTERO et al.,
2010; LUDWIG et al., 2004; NEPPLE et al., 2009). Além disso, em alguns casos
algumas complicações ocorrem em decorrência da utilização de uma bactéria viva,
levando ao aparecimento de sintomas como febre, cistite, pneumunites e, em casos
mais graves, sepse por BCG (LAMM, 1992; SUTTMANN et al., 2006).
Nesse sentido, algumas estratégias vem sendo desenvolvidas visando
melhorias para o tratamento de carcinomas superficiais de bexiga (SCHENKBRAAT; BANGMA, 2005). As mais utilizadas incluem: utilização de doses diminutas
da vacina; a administração de citocinas inflamatórias em conjunto com BCG;
identificação dos componentes micobacterianos responsáveis pela resposta
19
imunológica, evitando, assim, a utilização do bacilo vivo, o que diminuiria os riscos
de reações graves ou infecções; e a construção de cepas recombinantes (SCHENKBRAAT; BANGMA, 2005).
A construção de cepas recombinantes que proporcionem maior estímulo do
sistema imune e aumento do efeito antitumoral da bactéria constitui um dos
principais focos de pesquisas em melhorias imunoterapêuticas do BCG (AMIRKHAH
et al., 2009). Muitos avanços ocorreram nas últimas décadas no que diz respeito à
manipulação genética de micobactérias. Estes incluem o estabelecimento de
protocolos de transformação em micobactérias, geração de vetores bifuncionais
(shuttle vectors) para uso em E. coli e micobactéria, desenvolvimento de sistemas de
expressão diversos, incluindo diferentes promotores e sistemas de apresentação de
antígenos (JACOBS Jr. et al., 1987; SNAPPER et al., 1988; MATSUO et al., 1990).
Esses avanços permitiram a avaliação de BCG recombinante como veículo de
apresentação de antígenos heterólogos e vários estudos já demonstraram a
viabilidade do BCG em expressar antígenos heterólogos de diferentes espécies com
bastante êxito (O'DONNELL, 1997; OHARA; YAMADA, 2001; BASTOS et al, 2009).
O desenvolvimento de cepas recombinantes de BCG têm demonstrado que
essa estratégia é capaz de melhorar a eficácia da terapia para tumores de bexiga
(ANDRADE et al., 2010; LEE et al., 2004; LUO et al., 2004; LIN et al., 2012). Ensaios
realizados utilizando micobactéria recombinantes para citocinas constituem um dos
principais focos na busca por tratamentos mais eficientes para carcinomas in situ.
Estudos terapêuticos utilizando micobactéria e citocinas, principalmente IFN-α, IL-8,
IL-2 e IL-10, têm mostrado maior eficácia do que a utilização de citocinas sozinhas
ou de wtBCG (LUO et al., 2004, 2010, 2009, 2006, 2003, 2001), sendo a
combinação de BCG e IFN-α a mais promissora tanto para pacientes primários
quanto para aqueles que apresentam recidiva da doença após terapia com BCG
(LUO et al., 2001;LIU et al., 2009). A utilização de terapia combinada de BCG com
outras citocinas, como IL-2 e GM-CSF, tem apresentado resultados promissores
principalmente frente a tumores de pacientes inicialmente intolerantes ao BCG
(SCHENK-BRAAT; BANGMA, 2005).
A utilização de BCG recombinante para antígenos heterólogos de diferentes
bactérias, bem como a expressão de combinados antigênicos, também demonstram
eficácia aumentada frente a tumores, tanto em ensaios in vitro quanto em modelos
animais (CHUNG et al., 2003; ANDRADE et al., 2010). Chung et al (2003)
20
demonstraram que a co-expressão das proteínas MUC-1 e IL-2 por cepas de BCG
inibe a proliferação e o crescimento tumoral de carcinomas mamários em
camundongos. Cepas recombinantes de BCG expressando a toxina botulínica S1PT
se mostraram capazes de diminuir a proliferação de tumores de bexiga em modelos
murinos (ANDRADE et al., 2010). Ainda em modelos animais, a co-expressão por
BCG de antígeno Ag85B de M. tuberculosis, aliado a expressão de CFP10 e IL-2,
promove forte indução de resposta imune Th1 (LIN et al., 2012).
1.7 Antigeno Ag85B
O complexo AG85, composto pelas proteínas Ag85A, Ag85B e Ag85C, é o
principal antígeno compartilhado pelas cepas de M. bovis e M. tuberculosis (WIKER;
HARBOE, 1992). Estas proteínas são secretadas e retidas na parede celular das
micobactérias (WIKER; HARBOE, 1992) e são capazes de interagir especificamente
com fibronectinas (DENIS et al., 1997; NAITO et al., 1998).
Os primeiros relatos a respeito da eficácia de BCG recombinante para vacinas
de tuberculose foram explorados utilizando BCG superexpressando antígenos Ag85
(TRICCAS, 2010). Estes antígenos são capazes de conferir proteção contra
tuberculose em modelos animais e estão intimamente associados à infectividade da
bactéria (MUSTAFA et al., 1998). Por serem antígenos superexpressos, existem
evidências de que são capazes de aumentar a geração de peptídeos antigênicos,
bem como seus carregamentos subseqüentes para as moléculas de MHC II,
desencadeando processos imunológicos eficientes que podem levar a apoptose e a
autofagia (JAGANNATH et al., 2009).
21
2. OBJETIVOS
2.1 Geral
Aumentar a eficiência de imunoterapia para câncer superficial de bexiga
através da utilização de cepa auxotrófica de Mycobacterium bovis superexpressando
a proteína Antígeno 85B (Ag85B).
2.2 Específicos
1
Avaliar a regressão e/ou diminuição do crescimento tumoral in vitro da
linhagem celular de câncer superficial de bexiga, quando exposta a
presença de cepa recombinante de M. bovis ∆leuD;
2
Avaliação do perfil de expressão gênica da linhagem de carcinoma de
bexiga, para genes envolvidos em processos de apoptose e de ciclo
celular, após tratamento com cepa recombinante de M. bovis ∆leuD;
3
Avaliação da expressão gênica de enzimas antioxidantes pela linhagem de
carcinoma de bexiga, após tratamento com cepa recombinante de M. bovis
∆leuD;
4
Avaliação da presença de proteínas apoptóticas no sobrenadante da célula
em questão após tratamento com cepa recombinante de M. bovis ∆leuD.
22
3. ARTIGO
AUXOTROPHIC RECOMBINANT Mycobacterium bovis BCG OVEREXPRESSING
AG85B ENHANCES THE CYTOTOXICITY ON SUPERFICIAL BLADDER CANCER
CELLS IN VITRO
(Artigo científico escrito sob formato do periódico PLoS ONE)
(Submetido - Fator de Impacto 4.41)
23
AUXOTROPHIC RECOMBINANT Mycobacterium bovis BCG OVEREXPRESSING AG85B
ENHANCES THE CYTOTOXICITY ON SUPERFICIAL BLADDER CANCER CELLS IN VITRO
Karine Rech Begnini, Caroline Rizzi, Vinicius Farias Campos, Sibele Borsuk,
Eduarda Schultze, Virginia Yurgel, Fernanda Nedel, Odir Antônio Dellagostin, Tiago
Collares, Fabiana Kömmling Seixas*
Programa de Pós-Graduação em Biotecnologia (PPGB), Grupo de Pesquisa em
Oncologia Celular e Molecular, Laboratório de Genômica Funcional,
Biotecnologia/Centro de Desenvolvimento Tecnológico, Universidade Federal de
Pelotas, Pelotas, RS, Brazil
*Corresponding authors: Fabiana Kömmling Seixas, Universidade Federal de
Pelotas, Campus Universitário s/n, Capão do Leão, RS, Brazil, Cep: 96010-900.
Phone: 55 53 32757350
Fax: 55 53 32757354
E-mail: [email protected]
24
ABSTRACT
BCG therapy remains at the forefront of immunotherapy for treating patients
with superficial bladder cancer.
The high incidence of local side effects and
presence of non-responder diseases has led to efforts to improve the therapy.
Hence, we proposed that an auxotrophic recombinant BCG strain overexpressing
Ag85B (BCG ∆leuD/Ag85B), could enhance the cytotoxicity to human bladder
carcinoma cell line (5637). This rBCG was generated by incorporating of an
expression plasmid encoding the mycobacterial antigen Ag85B into BCG ∆leuD
strain. The inhibitory effect of BCG ∆leuD/Ag85B in 5637 cells was determined by the
MTT method, morphology observation and LIVE/DEAD assay. Gene expression
profiles for apoptotic genes, cell cycle-related genes and oxidative stress-related
genes were investigated by qRT-PCR. Bax, bcl-2 and p53 induction by BCG
∆leuD/Ag85B treatment was evaluated by Western blotting. BCG ∆leuD/Ag85B
revealed superior cytotoxicity effect than the strains used as control in this study. The
results shown that expression level of pro-apoptotic and cell cycle-related genes
increased after BCG ∆leuD/Ag85B treatment, whereas mRNA levels of antiapoptotic
genes decreased. Interestingly, BCG ∆leuD/Ag85B also increased the mRNA level of
antioxidant enzymes in bladder cancer cell line. Bax and p53 proteins levels were
increased by BCG ∆leuD/Ag85B treatment. In conclusion, these results suggested
that BCG ∆leuD/Ag85B enhances the cytotoxicity on superficial bladder cancer cells
in vitro. The therapeutic model using rBCG may have potential for future clinical
application to bladder cancer treatment.
Keywords: Bacillus Calmette-Guérin; recombinant BCG; superficial bladder cancer;
antitumor activity.
25
1. INTRODUCTION
Bladder cancer is the fourth most common cancer in men and eleventh most
common in women [1]. It’s a huge economic burden on the healthcare system and is
responsible for approximately 5% of all cancer deaths in humans [2]. Most of these
tumors are superficial at diagnosis and are treatable with surgical resection and local
prophylactic treatments [3]. Unfortunately, this disease recurs in up to 50% of these
patients despite surgery, and then this is potentially lethal [4]. Mycobacterium bovis
BCG-based therapy is the treatment of choice for superficial bladder cancer,
representing the only agent known to reduce progression into muscle-invasive
bladder cancer [5] and it is currently the most effective intravesical therapy for this
kind of tumor [3].
The anti-tumor effects of intravesical administration of M. bovis BCG in
bladder cancer was first described in 1976 by Morales et al [6]. Although BCG
therapy remains at the forefront of treating patients with superficial bladder cancer [7]
there are treatment failures, like BCG intolerant, refractory, resistant, and relapsing
disease [8]. The development of immunotherapy based on recombinant BCG (rBCG)
overexpressing antigens or expressing foreign antigens are a promising approach to
improve the performance of the BCG antitumor therapy [9] and current studies aim at
developing rBCG strains to further improve the effectiveness of the therapy [10–13].
The Ag85 complex, comprising of Ag85A, Ag85B and Ag85C proteins, are
major protective antigens shared by both BCG and M. tuberculosis [14]. These
proteins are secreted and retained in the cell wall of mycobacteria [14].
Overexpressed Ag85B elicits a strong Th1 response in vivo [15] and has been shown
that, in the cytosol of infected cells, it leads to the autophagic-lysosome pathway and
increases its presentation [16]. Mice vaccinated with rBCG overexpressing Ag85B
26
exhibit a robust immune response that is qualitatively superior to that elicited by
licensed BCG vaccine against tuberculosis [17]. In melanoma-bearing mice, Ag85B
antigen gene therapy induced the increase of serum IFN-gamma level in the animals,
inhibited the tumor growth and prolonged the survival of the mice [18].
The aim of this study was to verify the cytotoxicity effect of rBCG ∆leuD
overexpressing Ag85B in treating of human bladder carcinoma cell line (5637) and its
underlying mechanisms.
2. MATERIALS AND METHODS
2.1 Bacterial strains and cell culture
Three different BCG strains were used in this study: M. bovis BCG Pasteur,
which is very similar to the strain used in bladder cancer BCG-based therapy; M.
bovis BCG Pasteur ∆leuD, an auxotrophic strain for the leucine amino acid
developed by our research group [19]; and M. bovis BCG Pasteur ∆leuD/Ag85B
(rBCG), a recombinant BCG ∆leuD overexpressing Ag85B antigen. Strains were
grown on Middlebrook 7H9 medium (Difco Laboratories, Detroit, MI, USA)
supplemented with 0.5% glycerol, 0.05% Tween 80, and 10% oleic albumindextrose-catalase
(OADC)
or
on
solid
Middlebrook
7H10
medium
(Difco
Laboratories) supplemented with OADC. When required, the antibiotic kanamycin
was added to a final concentration of 25 µg/mL. Escherichia coli strain TOP10
(Invitrogen™, Carlsbad, CA, USA) was used for cloning and was grown in LuriaBertani medium at 37 °C with addition of kanamycin 50 µg/ml.
The human bladder carcinoma cells (5637) were obtained from Rio de Janeiro
Cell Bank (PABCAM, Federal University of Rio de Janeiro, RJ, Brazil). They were
cultured in Dulbecco’s modified Eagle’s medium (DMEM), supplemented with 10%
fetal bovine serum (FBS), 1% L-glutamine and 1% penicillin/streptomycin, purchased
27
respectively from Vitrocell Embriolife (Campinas, Brazil) and Gibco (Grand Island,
NY, USA). Cells were grown at 37°C in an atmosphere of 95% humidified air and 5%
CO2. The experiments were performed with cells and bacteria in the logarithmic
phase of growth and all experiments were run in triplicate.
2.2 Cloning Ag85b gene into mycobacterial expression vector
Coding sequences for Ag85b antigen was amplified from fbpB gene of M.
bovis genomic DNA. The primers used for fbpB gene PCR amplification were based
on
the
complete
M.
bovis
AF2122/97
GGGGTACCCGCTATGTAGCTCCAATTC-3’
genome
and
sequence
(5’5’-
GGGGTACCTCAGCCGGCGCC-3’), and were designed using Vector NTI 11.0
(Invitrogen™, Carlsbad, CA, USA). The M. bovis 30 kDa protein gene cassette,
consisting of the fbpB gene coding region and its endogenous promoter (1500 bp),
were obtained using standard PCR conditions and the enzyme Go TAq® Hot Start
Polymerase Sample (Promega). PCR product was digested with KpnI enzyme
(Promega), and inserted into pUP410 mycobacterial expression vector [19], which
had previously been digested with the same restriction enzyme. Competent E. coli
was then transformed with recombinant plasmid (pUP410::fbpB) and the clones were
checked by restriction enzyme digestion and PCR.
2.3 Construction of rBCG
Electrocompetent BCG Pasteur ΔleuD was transformed with pUP410::fbpB
and recombinant strains were selected in 7H10 media containing 25 µg/ml of
kanamycin. Recombinant BCG were grown to an optical density of 600 nm (OD600)
of 0.6 in selective 7H9 media and then 10 mL of culture was centrifuged (4000 g for
10 min), the pellet suspended in 1 mL of 100 mM Tris-HCl, pH 8.0, and cells were
28
lysed using a Ribolyser (Hybaid). The lysate was centrifuged (14000 g for 10 min)
and the supernatant recovered. Saturated ammonium sulfate solution was added to
supernatant to precipitate secreted recombinant protein, which was then collected by
centrifugation (4000 g for 10 min). Recombinant protein expression was assessed by
Western blot. BCG ΔleuD/Ag85B liquid culture was used for vaccine preparation.
2.4 Determination of cytotoxicity
The viability of 5637 cells was determined by measuring the reduction of soluble
MTT [3-(4,5-dimethylthiazol-2-yl)-2,5-diphe-nyltetrazolium bromide] to water insoluble
formazan [20]. Cells were seeded at a density of 2 x 10 4 cell per well in a volume of
100 µL in 96-well plates, and grown at 37°C in a 5% CO2 atmosphere for 24 h before
used in cell viability assay. Cells were then incubated with BCG strains (BCG Pasteur
or BCG ∆leuD or BCG ∆leuD/Ag85B) at a concentration of 4,8x106 CFU for 48 hours.
After incubation periods the media was removed and subsequently 180 µL of
medium and 20 µL MTT (5 mg MTT/mL solution) was added to each well. The plates
were incubated for an additional 2 h and medium was discarded. A volume of 200 µL
of DMSO was added to each well, and the formazan was solubilized on a shaker for
15 min at 150 rpm. The absorbance of each well was read on a microplate reader at
a test wavelength of 492 nm. Percent inhibition of cell proliferation was determinate
as follows: inhibitory growth = (1- Abs492treated cells/Abs492control cells) x 100%
[21]. All observations were validated by at least two independent experiments in
triplicates for each experiment.
2.5 Viability assessment and LIVE/DEAD assay
29
Cells were cultured and incubated with BCG strains as described above. At
the end of incubation period the cells were visualized with an inverted fluorescence
microscope Olympus IX71 (Olympus Optical Co., Ltd. Tokyo, Japan).
The LIVE/DEAD cell viability assay® (Invitrogen™, Carlsbad, CA, USA) was
conducted following the manufacturer's instructions. Live cells were able to take up
calcein and could be analyzed by green fluorescent light emission (488 nm).
Ethidium bromide homodimer diffuses through the permeable membrane of dead cell
and binds into their DNA. Dead cells could be detected by red fluorescent signal (546
nm). The LIVE/DEAD assay was analyzed with a fluorescence microscope Olympus
IX71 (Olympus Optical Co.) by multicolor imaging. The fluorescence emissions were
recorded as TIFF files using a digital camera (Nikon, Tokyo, Japan) attached to a
fluorescence microscope (DP 12; BX 51; Olympus, Tokyo, Japan) after excitation at
480 nm and emission at 510 nm. The recorded images was analyzed using Cell^F
software (Cell-F, New York, USA). The data were expressed as mean ± SEM of 6
observations in different fields with 100 cells in each field.
2.6 Quantitative Real-Time PCR (qRT-PCR)
Gene expression profiles for apoptotic genes, cell cycle-related genes and
oxidative stress-related genes were investigated by real-time PCR (qRT-PCR). Cells
were added in 6-well flat bottom plates at a density of 2 x 10 5 per well and grown at
37°C in a humidified atmosphere of 5% CO2/95% air for 24 h. The cells were then
incubated with BCG strains at a concentration of 4,8x10 7 for 48 h. After this period
the cells were washed with phosphate-buffered saline (PBS; Gibco) and RNA
extraction was performed. Total RNA extraction, cDNA synthesis and qRT-PCR were
conducted as previously describe [22]. Briefly, RNA samples were isolated using
30
TRIzol® Reagent (Invitrogen™) and samples were DNase-treated with a DNA-free®
kit (Ambion™, USA) following the manufacturer’s protocol. First-strand cDNA
synthesis was performed with 1 µg of RNA using High Capacity cDNA Reverse
Transcription kit (Applied Biosystems™, UK) according to the manufacturer’s
protocol. Real-time PCR reactions were run on a Stratagene® Mx3005P™ RealTime PCR System (Agilent Technologies, Santa Clara, CA, USA) using SYBR®
Green PCR Master Mix (Applied Biosystems™, UK) and using primers described in
Table 1.
2.7 Western blot
Cells (2x105 per well) were co-treated with BCG strains (4,8x107 CFU) for 48
h. Then they were pelleted by centrifugation, washed with PBS two times and
resuspended in 30µL of lysis buffer. Protein was electrophoresed for 2 h on 15%
SDS-polyacrylamide gels and then transferred to nitrocellulose membrane using an
electroblotter for 3 h. Membrane was blocked in 5% non-fat milk overnight and
probed with the primary antibody for p53, Bax and Bcl-2 (Sigma-Aldrich) for 1 h with
gentle agitation at room temperature. Antibodies rose against bcl-2 (1:2000), p53
(1:2000) and bax (1:2000) (Cell Signaling Biotech) was diluted in PBST. The blots
were washed for three times with PBST and incubated with an anti-mouse antibody
conjugated to horseradish peroxidase (Sigma-Aldrich) 1:1000 dilutions in PBST for 1
h. After three successive washes with PBST, a chromogenic substrate was used for
protein detection.
2.8 Data analysis
31
Data sets were analyzed using one-way ANOVA followed by a Tukey test for
multiple comparisons. Significance was considered at P<0.05 in all analyses. Data
were expressed as mean ± SEM.
3. RESULTS
3.1 Construction and Ag85B overexpression of recombinant BCG
The construction used in this study was confirmed by PCR and restriction site
analysis (data not shown). The Ag85B gene coding sequence was incorporated
immediately downstream of Ag85B signal sequence. Recombinant protein was
readily detectable in rBCG ΔleuD lysates and culture supernatant by Western blot
using polyclonal anti-Ag85 antibody (Fig.1A). Both cytoplasm and secreted
recombinant protein presented 30 kDa of molecular mass.
3.2 BCG ∆leuD/Ag85B inhibits cell proliferation of human bladder carcinoma cells
Human bladder carcinoma cells were incubated with BCG strains (BCG
Pasteur or BCG ∆leuD or BCG ∆leuD/Ag85B) for 48 h. As demonstrated in Fig. 1B,
an auxotrophic recombinant BCG strain overexpressing Ag85B (BCG ∆leuD/Ag85B)
demonstrated a significant in vitro cytotoxic activity after 48 h of treatment, inhibiting
more than 50% of tumor cells. Percent inhibition of cell proliferation for BCG
∆leuD/Ag85B was 77.8% while for the other strains it was 28% (BCG ∆leuD) and
38.1% (BCG Pasteur). This result suggests that BCG ∆leuD/Ag85B is more effective
against bladder cancer cells in vitro than BCG ∆leuD or BCG Pasteur strains
(P<0.05).
The viability assessment of untreated and treated cells with BCG Pasteur;
BCG ∆leuD and BCG ∆leuD/Ag85B at 48 h of treatment was observed. Cell density
32
in the control group (untreated) was greater than that in the treated groups, however
no additional alterations were observed in the treatment groups (supplementary
data).
3.3 BCG ∆leuD/Ag85B increased 5637 cell death
The LIVE/DEAD assay was carried out to evaluate cell viability using a twocolor fluorescence approach. Figure 2 shows a histogram analysis of the red channel
for quantitative analysis of cell death. BCG ∆leuD/Ag85B treatment (Fig. 2C)
promotes an increase in cell death (red fluorescence), when compared to control
(Fig. 2A). BCG Pasteur (Fig. 2B) treatment promotes cell death similarly to the
control group. Additionally, BCG strains remained alive after 48 h of co-culture with
5637 cell line what is necessary for a successful BCG therapy (Fig. 2D).
3.4 Ag85B BCG overexpression changes apoptotic gene expression profile
Expression of anti-apoptotics genes bcl-2 and survivin and pro-apoptotic bax
were evaluated, as well as of apoptosis-inducing factor (AIF) and Endonuclease G
(Endo G) genes. Bcl-2 and survivin mRNA levels were decreased (P<0.05) in cells
exposed to BCG ∆leuD/Ag85B compared to control (Fig. 3A). mRNA expression from
cells treated with BCG ∆leuD /Ag85B was lower (P<0.05) than those treated with
BCG Pasteur and BCG ∆leuD for both antiapoptotic genes. Moreover, bax mRNA
levels were higher (P<0.05) in cells exposed to BCG ∆leuD/Ag85B (Fig. 3B)
compared to not treated cells and to BCG Pasteur and BCG ∆leuD treated cells.
Apoptosis-Inducing Factor (AIF) mRNA expression was up-regulated in BCG
∆leuD/Ag85B treated cells (P<0.05) when compared to control and to the other
treatments (Fig. 3B). No differences between control and BCG Pasteur or BCG
∆leuD treatment were observed in bcl-2, survivin, bax and AIF gene expression.
33
Endo G mRNA level was significantly higher (P<0.05) in BCG ∆leuD/Ag85B and BCG
∆leuD treatments compared to control and to BCG Pasteur treatment (Fig. 3B).
However, no difference between the BCG ∆leuD/Ag85B and BCG ∆leuD treatment
was observed. Bax/bcl-2 ratio also changes after BCG ∆leuD/Ag85B treatment (Fig.
4). Bax/bcl-2 ratio increased 6 folds in 5637 cells exposed to BCG ∆leuD/Ag85B
compared to not treat cells and to BCG Pasteur and BCG ∆leuD treated cells.
The BCG ∆leuD overexpressing Ag85B also induced changes in mRNA
expression of caspases in 5637 cells. Initiator capase-8 and caspase-9 were upregulated (P<0.05) by BCG ∆leuD/Ag85B compared to control cells and to BCG
Pasteur and BCG ∆leuD treatments (Fig. 5B and C). Additionally, caspase-8 was upregulated 2-fold compared to other treatments. Cells treated with BCG ∆leuD/Ag85B
for 48 h also showed significantly higher mRNA level of the executioner caspase-3
(P<0.05) compared to untreated cells and to BCG Pasteur and BCG ∆leuD
treatments (Fig. 5A). No differences between control and BCG Pasteur or BCG
∆leuD treatment were observed in caspase-8, caspase-9 and caspase-3 gene
expression.
3.5 BCG ∆leuD/Ag85B changes gene expression in 5637 cells for antioxidant
enzymes
Antioxidant enzymes gene expression profiles were also analyzed. The
enzymes catalase (CAT), Cu/Zn superoxide dismutase (Cu/Zn-SOD), manganese
superoxide dismutase (Mn-SOD), glutathione peroxidase (GPx), glutathione-Stransferase (GST) and Thioredoxin reductase-1 (TRX) were investigated in this
study. CAT, Cu/Zn-SOD, GPx and Mn-SOD mRNA levels were increased (P<0.05)
in cells exposed to BCG ∆leuD/Ag85B compared to control (Fig. 6A). The mRNA
34
expression from cells treated with BCG ∆leuD /Ag85B was up-regulated (P<0.05)
compared to those treated with BCG Pasteur and BCG ∆leuD for GPx, Mn-SOD and
Cu/Zn-SOD antioxidant enzymes; however there was no difference between BCG
∆leuD and BCG ∆leuD/Ag85B treatments in CAT mRNA expression (Fig. 6A). No
differences between control and BCG Pasteur or BCG ∆leuD treatment were
observed in CAT, Cu/Zn-SOD, GPx and Mn-SOD gene expression. Moreover, GST
and TRX mRNA expression pattern was investigated and no differences between
treated and untreated cells were observed (Fig. 6B).
3.6 BCG ∆leuD/Ag85B changes cell cycle-related gene expression in 5637 cells
In comparison to controls, 5637 tumor cells treated with BCG ∆leuD/Ag85B
showed an up-regulated p53 expression (P<0.05), while no difference was observed
between BCG Pasteur and BCG ∆leuD treatments to untreated tumor cells (Fig. 7).
The p21 expression showed a similar pattern to p53 expression, and BCG
∆leuD/Ag85B induced an increase (P<0.05) in p21 mRNA level (Fig 7) compared to
other treatments and to untreated 5637 cells.
3.7 Bax and p53 protein increased by BCG ∆leuD/Ag85B treatment in 5637 cells
Bax and p53 proteins levels were increased by BCG ∆leuD/Ag85B treatment
at 48 h time point. On the contrary, BCG Pasteur and BCG ∆leuD treatments showed
a weak expression of bax and p53 protein in 5637 cells. No bcl-2 protein change was
observed in 5637 treated and untreated cells (data not shown).
35
4. DISCUSSION
Mycobacterium bovis bacille Calmette–Guerin (BCG) is one of the great
success stories of immunotherapy as a treatment for superficial urothelial carcinoma
of the bladder [23]. The high incidence of local side effects and presence of nonresponders to the cancer treatment has led to efforts to improve the therapeutic
vaccine. The prospect of genetically modifying BCG’s properties to create a more
specific cancer vaccine with inclusion of tumor-associated antigens is a reality [24]
and rBCG strains are capable of improving the effectiveness of the therapy [10–13].
To the best of our knowledge, this is the first investigation on the possibility of using
an auxotrophic BCG strain overexpressing Ag85B (BCG ∆leuD/Ag85B) to therapy for
bladder cancer. BCG has the potential to be an effective live vector for multivalent
vaccines and antitumor therapies. However, most mycobacterial cloning vectors rely
on antibiotic resistance genes as selectable markers, which would be undesirable in
any practical therapies [19]. In this study, we used an auxotrophic complementation
as a selectable marker that would be suitable for use in clinical therapy.
Successful BCG therapy requires immune system activation, however in vitro
studies showed that some BCG strains act directly on tumour cells inhibiting the
proliferation through apoptosis [25]. Herein, we demonstrated an increased
cytotoxicity in bladder cancer cell line (5637) induced by an rBCG strain
overexpressing Ag85B. The secreted Ag85B protein has been the focus of intensive
research in recent years. It has been shown that Ag85B possess the ability to
specifically interact with fibronectin (Fn) proteins [26,27]. Since Fn binding proteins
are likely to be important virulence factors of mycobacteria and adhesion is a pivotal
first step that allows pathogenicity, Ag85B plays a critical role in mycobacteria
adherence to host cells, initiating infection, and may contribute to the invasion and
36
dissemination of mycobacteria in host tissue [28]. Our results indicate that Ag85B
might serve as an important colonization factor potentially contributing to
mycobacterial virulence, what may be related with increased cytotoxicity and cell
death in bladder cancer cell line in vitro.
Moreover, Ag85B is an antigen strongly recognized by T-cell in the first phase
of mycobacterial infection [30]. Many studies demonstrated a protective action
against tuberculosis induced by recombinant Ag85B BCG vaccines in animal [29–31]
and human models [32]. In addition, immunogenicity study showed that rBCG
overexpressing Ag85B enhances immunogenicity of BCG and induces a robust and
lasting immune response [16]. These support our speculation that our BCG
∆leuD/Ag85B will conduct tumour suppression by direct killing effect to bladder
cancer cells and may trigger a strong subsequent immune response when used as
an immuno-therapeutic agent against bladder cancer.
Tumor suppression frequently involves the modulation of signal transduction
pathways, leading to alterations in gene expression, arrest in cell cycle progression
or apoptosis [33]. Apoptosis is considered a highly regulated process that allows a
cell to self-degrade in order to eliminate an unwanted or dysfunctional cell [34].
Conventional anticancer treatments, such as chemotherapy and radiotherapy, kill
tumor cells primarily by the induction of apoptosis through activation of the intrinsic
pathway [34]. The intrinsic apoptotic pathway is mediated by the mitochondria and is
mainly controlled by the balance and interactions between pro- and antiapoptotic
members of the Bcl-2 family proteins, which regulate the permeability of the
mitochondrial membrane [35]. It has been proposed that the ratio between bcl-2 and
bax genes is more important in the regulation of apoptosis than the level of each bcl2 family protein alone [36]. Our data indicated that treatment with BCG ∆leuD/Ag85B
37
markedly decreased the mRNA levels of bcl-2 and increased bax expression, while
opposite results were observed in BCG Pasteur treatment. So, the bax/bcl-2 ratio
increased with the treatment of BCG ∆leuD/Ag85B in 5637 cell line what may be an
evidential that Bax and Bcl-2 are involved in apoptotic events associated with the
cytotoxic effects of rBCG treatment.
Caspases play a central role in apoptosis [37]. Once activated, bax promotes
cytochrome c release and mitochondrial fission, which leads to the activation of
APAF1 into an apoptosome and activates caspase-9 to activate caspase-3.
Caspase-8 is activated by the extrinsic apoptosis pathway however it also leads to
caspase-3 activation [38]. When activated, caspases cleave a series of substrates,
activate DNases and orchestrate cell death and its removal by scavenger
macrophages [35]. A sharp increase in caspase-3 activity might be sufficient to
trigger the induction of an irreversible death program [39]. In addition to higher
bax/bcl-2 ratio, our results also showed an increased in mRNA level of caspase-3,
caspase-9 and caspase-8, suggesting involvement of caspases with the cytotoxic
effects associated with BCG ∆leuD/Ag85B treatment.
In 5637 cells, BCG ∆leuD/Ag85B also modulates the expression of
Endonuclease G (Endo G) and AIF genes, which were substantially up-regulated at
mRNA level in this study. A hallmark of apoptosis is the fragmentation of nuclear
DNA and evidence exists that DNA fragmentation can occur independently of
caspase activity [40]. Apoptosis-inducing factor (AIF) is a flavoprotein that resides in
the mitochondrial intermembrane space. Upon induction of apoptosis, AIF
translocates from the mitochondria to the nucleus and causes chromatin
condensation and large-scale DNA fragmentation [41]. Endo G is a mitochondrial
nuclease that is released under apoptotic conditions and plays a role in nuclear DNA
38
fragmentation [40]. Interestingly, both genes cause DNA fragmentation independently
of caspases activation [40,42,43], indicating that apoptosis can proceed in the
absence of caspase activity [38]. The apoptosis gene expression data from our
experiments confirms the results of cytotoxicity assay, showing that Ag85B
overexpressing by BCG may induces apoptosis in 5637 cells and these effect may
occur by activation of different apoptosis pathways.
Checkpoints are control mechanisms that ensure the proper timing of cell
cycle events by enforcing the dependency of late events on the completion of early
events [44]. Entry into mitosis is blocked by the G2 checkpoint mechanism when
DNA is damaged [45]. The cell cycle at G2/M phase is arrested by p53 via the
lowering of cyclin B1 levels [46,47]. Furthermore, several investigators have noted
that cells deficient in p21 escape of the G2/M phase cell cycle arrest when exposed
to DNA-damaging agents [48]. We demonstrate here that BCG ∆leuD/Ag85B
increased the expression of p53 and p21 and thus potentially may be effective as an
anti-proliferative agent for 5637 cells, through maintenance of G2/M cell cycle arrest.
Reactive oxygen species (ROS) can influence cell proliferation, gene
regulation and cell death [49]. Epithelial cells can internalize bacteria and produce
ROS after bacterial internalization [50]. Thus, ROS may have a significant role in
determining the clinical outcome of BCG treatment [51]. As shown in this study, the
overexpression of Ag85B also increased the mRNA level of antioxidant enzymes
(CAT, Cu/Zn-SOD, GPx and Mn-SOD) in bladder cancer cells line after BCG
∆leuD/Ag85B treatment. The well established role of antioxidant enzymes against
cancer is to prevent oxidative DNA damage [52]. However, some newly understood
mechanisms also exist. Overexpression of CAT has been found to delay G0/G1 to Sphase transition during cell cycle progression in mouse aortic endothelial cells [53]. In
39
a study using animal model, gene therapy using a combination of GPx and Mn-SOD
slowed suppressed tumor growth by 81% and increased animal survival [54].
Moreover, the anticancer activity of Ginkgo biloba extract is supposed to be due to
the increasing activity of antioxidant enzymes, including SOD and CAT [55]. Future
works need to be carried out, however the increased antioxidant enzymes mRNA
levels in the present study might reflect the response of cells toward death.
In conclusion, our findings indicate that BCG ∆leuD/Ag85B enhances the
cytotoxicity on superficial bladder cancer cells in vitro and this effect may occur by
apoptosis and cell-cycle arrest. Additionally, we speculate that BCG ∆leuD/Ag85B
might be superior therapeutic agent to bladder cancer than the now common
commercially available strains.
ACKNOWLEDGMENTS
This work was supported by the Brazilian funding agencies CAPES, CNPq
and FAPERGS.
AUTHOR CONTRIBUTIONS
Conceived and designed the experiments: KRB CR FN. Performed the experiments:
KRB
CR
VY
ES.
Analyzed
the
data:
KRB
VFC.
Contributed
reagents/materials/analysis tools: OAD TC FS. Wrote the paper: KRB FS.
Contributed intellectually and read and approved the final manuscript: KRB SB TC
OAD FS.
Competing interests: The authors have no conflict of interest.
40
REFERENCES
1. Siegel R, Ward E, Brawley O, Jemal A (2011) Cancer statistics, 2011: the
impact of eliminating socioeconomic and racial disparities on premature
cancer deaths. CA Cancer J Clin 61: 212-236. caac.20121
[pii];10.3322/caac.20121 [doi].
2. Simons MP, Nauseef WM, Griffith TS (2007) Neutrophils and TRAIL: insights
into BCG immunotherapy for bladder cancer. Immunol Res 39: 79-93.
IR:39:1-3:79 [pii].
3. Gontero P, Bohle A, Malmstrom PU, O'Donnell MA, Oderda M, Sylvester R,
Witjes F (2010) The role of bacillus Calmette-Guerin in the treatment of
non-muscle-invasive bladder cancer. Eur Urol 57: 410-429. S03022838(09)01165-8 [pii];10.1016/j.eururo.2009.11.023 [doi].
4. Cookson MS, Herr HW, Zhang ZF, Soloway S, Sogani PC, Fair WR (1997)
The treated natural history of high risk superficial bladder cancer: 15year outcome. J Urol 158: 62-67. S0022-5347(01)64597-X
[pii];10.1097/00005392-199707000-00017 [doi].
5. Sylvester RJ, van der MEIJDEN AP, Lamm DL (2002) Intravesical bacillus
Calmette-Guerin reduces the risk of progression in patients with
superficial bladder cancer: a meta-analysis of the published results of
randomized clinical trials. J Urol 168: 1964-1970.
10.1097/01.ju.0000034450.80198.1c [doi];S0022-5347(05)64273-5 [pii].
6. Morales A, Eidinger D, Bruce AW (1976) Intracavitary Bacillus CalmetteGuerin in the treatment of superficial bladder tumors. J Urol 116: 180183.
7. Ludwig AT, Moore JM, Luo Y, Chen X, Saltsgaver NA, O'Donnell MA, Griffith
TS (2004) Tumor necrosis factor-related apoptosis-inducing ligand: a
novel mechanism for Bacillus Calmette-Guerin-induced antitumor
activity. Cancer Res 64: 3386-3390. 10.1158/0008-5472.CAN-04-0374
[doi];64/10/3386 [pii].
8. Nepple KG, Aubert HA, Braasch MR, O'Donnell MA (2009) Combination of
BCG and interferon intravesical immunotherapy: an update. World J
Urol 27: 343-346. 10.1007/s00345-009-0429-6 [doi].
9. Amirkhah R, Khanahmad H, Abolhassani M, Pooya M, Movassagh H,
Shokrgozar MA (2009) Improvement of bladder cancer immunotherapy
by creating a recombinant Bacille Calmette-Gu'erin which secrets p53
protein. Med Hypotheses 72: 754. S0306-9877(09)00067-X
[pii];10.1016/j.mehy.2009.01.035 [doi].
10. Andrade PM, Chade DC, Borra RC, Nascimento IP, Villanova FE, Leite LC,
Andrade E, Srougi M (2010) The therapeutic potential of recombinant
BCG expressing the antigen S1PT in the intravesical treatment of
41
bladder cancer. Urol Oncol 28: 520-525. S1078-1439(08)00388-8
[pii];10.1016/j.urolonc.2008.12.017 [doi].
11. Yu DS, Lee CF, Hsieh DS, Chang SY (2004) Antitumor effects of recombinant
BCG and interleukin-12 DNA vaccines on xenografted murine bladder
cancer. Urology 63: 596-601. 10.1016/j.urology.2003.09.039
[doi];S0090429503010276 [pii].
12. Lee CF, Chang SY, Hsieh DS, Yu DS (2004) Treatment of bladder carcinomas
using recombinant BCG DNA vaccines and electroporative gene
immunotherapy. Cancer Gene Ther 11: 194-207.
10.1038/sj.cgt.7700658 [doi];7700658 [pii].
13. Luo Y, Yamada H, Chen X, Ryan AA, Evanoff DP, Triccas JA, O'Donnell MA
(2004) Recombinant Mycobacterium bovis bacillus Calmette-Guerin
(BCG) expressing mouse IL-18 augments Th1 immunity and
macrophage cytotoxicity. Clin Exp Immunol 137: 24-34. 10.1111/j.13652249.2004.02522.x [doi];CEI2522 [pii].
14. Wiker HG, Harboe M (1992) The antigen 85 complex: a major secretion
product of Mycobacterium tuberculosis. Microbiol Rev 56: 648-661.
15. Ariga H, Shimohakamada Y, Nakada M, Tokunaga T, Kikuchi T, Kariyone A,
Tamura T, Takatsu K (2007) Instruction of naive CD4+ T-cell fate to Tbet expression and T helper 1 development: roles of T-cell receptormediated signals. Immunology 122: 210-221. IMM2630
[pii];10.1111/j.1365-2567.2007.02630.x [doi].
16. Jagannath C, Lindsey DR, Dhandayuthapani S, Xu Y, Hunter RL, Jr., Eissa
NT (2009) Autophagy enhances the efficacy of BCG vaccine by
increasing peptide presentation in mouse dendritic cells. Nat Med 15:
267-276. nm.1928 [pii];10.1038/nm.1928 [doi].
17. Lin CW, Su IJ, Chang JR, Chen YY, Lu JJ, Dou HY (2012) Recombinant BCG
coexpressing Ag85B, CFP10, and interleukin-12 induces multifunctional
Th1 and memory T cells in mice. APMIS 120: 72-82. 10.1111/j.16000463.2011.02815.x [doi].
18. Wu XZ, Wei HM, Zheng XD, Jin TC, Tian ZG (2007) [Induction and
mechanism study of anti-melanoma immune response by M.
tuberculosis Ag85B]. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi 23: 36-38.
19. Borsuk S, Mendum TA, Fagundes MQ, Michelon M, Cunha CW, McFadden J,
Dellagostin OA (2007) Auxotrophic complementation as a selectable
marker for stable expression of foreign antigens in Mycobacterium
bovis BCG. Tuberculosis (Edinb ) 87: 474-480. S1472-9792(07)00087X [pii];10.1016/j.tube.2007.07.006 [doi].
20. Ali D, Ray RS, Hans RK (2010) UVA-induced cyototoxicity and DNA damaging
potential of benz (e) acephenanthrylene. Toxicol Lett 199: 193-200.
S0378-4274(10)01674-7 [pii];10.1016/j.toxlet.2010.08.023 [doi].
42
21. Zheng D, Wang Y, Zhang D, Liu Z, Duan C, Jia L, Wang F, Liu Y, Liu G, Hao
L, Zhang Q (2011) In vitro antitumor activity of silybin nanosuspension
in PC-3 cells. Cancer Lett 307: 158-164. S0304-3835(11)00189-3
[pii];10.1016/j.canlet.2011.03.028 [doi].
22. Campos VF, Collares T, Deschamps JC, Seixas FK, Dellagostin OA, Lanes
CF, Sandrini J, Marins LF, Okamoto M, Sampaio LA, Robaldo RB
(2010) Identification, tissue distribution and evaluation of brain
neuropeptide Y gene expression in the Brazilian flounder Paralichthys
orbignyanus. J Biosci 35: 405-413.
23. Kresowik TP, Griffith TS (2009) Bacillus Calmette-Guerin immunotherapy for
urothelial carcinoma of the bladder. Immunotherapy 1: 281-288.
10.2217/1750743X.1.2.281 [doi].
24. O'Donnell MA (2009) Optimizing BCG therapy. Urol Oncol 27: 325-328.
S1078-1439(08)00318-9 [pii];10.1016/j.urolonc.2008.10.024 [doi].
25. Schwarzer K, Foerster M, Steiner T, Hermann IM, Straube E (2010) BCG
strain S4-Jena: An early BCG strain is capable to reduce the
proliferation of bladder cancer cells by induction of apoptosis. Cancer
Cell Int 10: 21. 1475-2867-10-21 [pii];10.1186/1475-2867-10-21 [doi].
26. Denis O, Lozes E, Huygen K (1997) Induction of cytotoxic T-cell responses
against culture filtrate antigens in Mycobacterium bovis bacillus
Calmette-Guerin-infected mice. Infect Immun 65: 676-684.
27. Naito M, Ohara N, Matsumoto S, Yamada T (1998) The novel fibronectinbinding motif and key residues of mycobacteria. J Biol Chem 273:
2905-2909.
28. Kuo CJ, Bell H, Hsieh CL, Ptak CP, Chang YF (2012) Novel mycobacteria
antigen 85 complex binding motif on fibronectin. J Biol Chem 287:
1892-1902. M111.298687 [pii];10.1074/jbc.M111.298687 [doi].
29. Roche PW, Triccas JA, Avery DT, Fifis T, Billman-Jacobe H, Britton WJ (1994)
Differential T cell responses to mycobacteria-secreted proteins
distinguish vaccination with bacille Calmette-Guerin from infection with
Mycobacterium tuberculosis. J Infect Dis 170: 1326-1330.
30. Mustafa AS, Amoudy HA, Wiker HG, Abal AT, Ravn P, Oftung F, Andersen P
(1998) Comparison of antigen-specific T-cell responses of tuberculosis
patients using complex or single antigens of Mycobacterium
tuberculosis. Scand J Immunol 48: 535-543.
31. Wang J, Qie Y, Zhu B, Zhang H, Xu Y, Wang Q, Chen J, Liu W, Wang H
(2009) Evaluation of a recombinant BCG expressing antigen Ag85B
and PPE protein Rv3425 from DNA segment RD11 of Mycobacterium
tuberculosis in C57BL/6 mice. Med Microbiol Immunol 198: 5-11.
10.1007/s00430-008-0098-x [doi].
43
32. Hoft DF, Blazevic A, Abate G, Hanekom WA, Kaplan G, Soler JH, Weichold F,
Geiter L, Sadoff JC, Horwitz MA (2008) A new recombinant bacille
Calmette-Guerin vaccine safely induces significantly enhanced
tuberculosis-specific immunity in human volunteers. J Infect Dis 198:
1491-1501. 10.1086/592450 [doi].
33. Yun JM, Kweon MH, Kwon H, Hwang JK, Mukhtar H (2006) Induction of
apoptosis and cell cycle arrest by a chalcone panduratin A isolated from
Kaempferia pandurata in androgen-independent human prostate
cancer cells PC3 and DU145. Carcinogenesis 27: 1454-1464. bgi348
[pii];10.1093/carcin/bgi348 [doi].
34. Vangestel C, Van De Wiele C, Mees G, Peeters M (2009) Forcing cancer cells
to commit suicide. Cancer Biother Radiopharm 24: 395-407.
10.1089/cbr.2008.0598 [doi].
35. Youle RJ, Strasser A (2008) The BCL-2 protein family: opposing activities that
mediate cell death. Nat Rev Mol Cell Biol 9: 47-59. nrm2308
[pii];10.1038/nrm2308 [doi].
36. Gajewski TF, Thompson CB (1996) Apoptosis meets signal transduction:
elimination of a BAD influence. Cell 87: 589-592. S00928674(00)81377-X [pii].
37. Huang TC, Huang HC, Chang CC, Chang HY, Ou CH, Hsu CH, Chen ST,
Juan HF (2007) An apoptosis-related gene network induced by novel
compound-cRGD in human breast cancer cells. FEBS Lett 581: 35173522. S0014-5793(07)00724-7 [pii];10.1016/j.febslet.2007.06.067 [doi].
38. Wang X (2001) The expanding role of mitochondria in apoptosis. Genes Dev
15: 2922-2933.
39. Gu D, Tonthat NK, Lee M, Ji H, Bhat KP, Hollingsworth F, Aldape KD,
Schumacher MA, Zwaka TP, McCrea PD (2011) Caspase-3 cleavage
links delta-catenin to the novel nuclear protein ZIFCAT. J Biol Chem
286: 23178-23188. M110.167544 [pii];10.1074/jbc.M110.167544 [doi].
40. van LG, Schotte P, van GM, Demol H, Hoorelbeke B, Gevaert K, Rodriguez I,
Ruiz-Carrillo A, Vandekerckhove J, Declercq W, Beyaert R,
Vandenabeele P (2001) Endonuclease G: a mitochondrial protein
released in apoptosis and involved in caspase-independent DNA
degradation. Cell Death Differ 8: 1136-1142. 10.1038/sj.cdd.4400944
[doi].
41. Susin SA, Lorenzo HK, Zamzami N, Marzo I, Snow BE, Brothers GM, Mangion
J, Jacotot E, Costantini P, Loeffler M, Larochette N, Goodlett DR,
Aebersold R, Siderovski DP, Penninger JM, Kroemer G (1999)
Molecular characterization of mitochondrial apoptosis-inducing factor.
Nature 397: 441-446. 10.1038/17135 [doi].
42. Miramar MD, Costantini P, Ravagnan L, Saraiva LM, Haouzi D, Brothers G,
Penninger JM, Peleato ML, Kroemer G, Susin SA (2001) NADH
44
oxidase activity of mitochondrial apoptosis-inducing factor. J Biol Chem
276: 16391-16398. 10.1074/jbc.M010498200 [doi];M010498200 [pii].
43. Li LY, Luo X, Wang X (2001) Endonuclease G is an apoptotic DNase when
released from mitochondria. Nature 412: 95-99. 10.1038/35083620
[doi];35083620 [pii].
44. Hartwell LH, Weinert TA (1989) Checkpoints: controls that ensure the order of
cell cycle events. Science 246: 629-634.
45. Taylor WR, Stark GR (2001) Regulation of the G2/M transition by p53.
Oncogene 20: 1803-1815. 10.1038/sj.onc.1204252 [doi].
46. Hu L, Sun Y, Hu J (2010) Catalpol inhibits apoptosis in hydrogen peroxideinduced endothelium by activating the PI3K/Akt signaling pathway and
modulating expression of Bcl-2 and Bax. Eur J Pharmacol 628: 155163. S0014-2999(09)01098-X [pii];10.1016/j.ejphar.2009.11.046 [doi].
47. Gochhait S, Dar S, Pal R, Gupta P, Bamezai RN (2009) Expression of DNA
damage response genes indicate progressive breast tumors. Cancer
Lett 273: 305-311. S0304-3835(08)00651-4
[pii];10.1016/j.canlet.2008.08.009 [doi].
48. Tsujimoto Y, Croce CM (1986) Analysis of the structure, transcripts, and
protein products of bcl-2, the gene involved in human follicular
lymphoma. Proc Natl Acad Sci U S A 83: 5214-5218.
49. Gamaley IA, Klyubin IV (1999) Roles of reactive oxygen species: signaling
and regulation of cellular functions. Int Rev Cytol 188: 203-255.
50. Kim JM, Eckmann L, Savidge TC, Lowe DC, Witthoft T, Kagnoff MF (1998)
Apoptosis of human intestinal epithelial cells after bacterial invasion. J
Clin Invest 102: 1815-1823. 10.1172/JCI2466 [doi].
51. Pook SH, Esuvaranathan K, Mahendran R (2002) N-acetylcysteine augments
the cellular redox changes and cytotoxic activity of internalized
Mycobacterium bovis in human bladder cancer cells. J Urol 168: 780785. S0022-5347(05)64744-1 [pii].
52. Khan A, Tania M, Zhang D, Chen H (2010) Antioxidant Enzymes and Cancer.
Chin J Cancer Res 22: 87-92.
53. Onumah OE, Jules GE, Zhao Y, Zhou L, Yang H, Guo Z (2009)
Overexpression of catalase delays G0/G1- to S-phase transition during
cell cycle progression in mouse aortic endothelial cells. Free Radic Biol
Med 46: 1658-1667. S0891-5849(09)00178-6
[pii];10.1016/j.freeradbiomed.2009.03.018 [doi].
54. Liu J, Hinkhouse MM, Sun W, Weydert CJ, Ritchie JM, Oberley LW, Cullen JJ
(2004) Redox regulation of pancreatic cancer cell growth: role of
glutathione peroxidase in the suppression of the malignant phenotype.
Hum Gene Ther 15: 239-250. 10.1089/104303404322886093 [doi].
45
55. Feng X, Zhang L, Zhu H (2009) Comparative anticancer and antioxidant
activities of different ingredients of Ginkgo biloba extract (EGb 761).
Planta Med 75: 792-796. 10.1055/s-0029-1185451 [doi].
46
Table 1: Primers used in the study.
Gene
Sequence 5’- 3’
Gene
Sequence 5’- 3’
p53 For
AGCGAGCACTGCCCAACA
AIF For
GGGAGGACTACGGCAAAGGT
p53 Rev
CACGCCCACGGATCTGAA
AIF Rev
CTTCCTTGCTATTGGCATTCG
P21 For
CCTAATCCGCCCACAGGAA
CuZn-SOD For
AGGGCATCATCAATTTCGAG
P21 Rev
ACCTCCGGGAGAGAGGAAAA
Cuzn-SOD Rev
TGCCTCTCTTCATCCTTTGG
Bcl-2 For
GTGTGGAGAGCGTCAACC
Mn-SOD For
GGAAGCCATCAAACGTGACT
Bcl-2 Rev
CTTCAGAGACAGCCAGGAG
Mn-SOD Rev
CTGATTTGGACAAGCAGCAA
Survivin For
CTGTGGGCCCCTTAGCAAT
CAT For
TTTCCCAGGAAGATCCTGAC
Survivin Rev
TAAGCCCGGGAATCAAAACA
CAT Rev
ACCTTGGTGAGATCGAATGG
Bax For
ATGCGTCCACCAAGAAGC
GPx For
TTCCCGTGCAACCAGTTTG
Bax Rev
ACGGCGGCAATCATCCTC
GPx Rev
TTCACCTCGCACTTCTCGAA
Caspase-3 For
CAGTGGAGGCCGACTTCTTG
GST For
CCCGATGTATCACGCAGTTA
Caspase-3 Rev
TGGCACAAAGCGACTGGAT
GST Rev
TTCACTGCAACAGCAAAACC
Caspase-8 For
GGATGGCCACTGTGAATAACTG
TRX For
CTTGTGGCCTTTCTGAGGAG
Caspase-8 Rev
TCGAGGACATCGCTCTCTCA
TRX Rev
CTCTTGACGGAATCGTCCAT
Caspase-9 For
CCAGAGATTCGCAAACCAGAGG
GAPDH For
GGATTTGGTCGTATTGGG
Caspase-9 Rev
GAGCACCGACATCACCAAATCC
GAPDH Rev
TCGCTCCTGGAAGATGG
Endo G For
GTACCAGGTCATCGGCAAGAA
Ag85B For
GGGGTACCCGCTATGTAGCTCCAATTC
Endo G Rev
CGTAGGTGCGGAGCTCAATT
Ag85B Rev
GGGGTACCTCAGCCGGCGCC
47
Figure 1: Ag85B overexpression in BCG ∆leuD. (A) Lysates and supernatants were
subjected to western blot analysis for Ag85B antibodies. (1) BCG ∆leuD/Ag85B supernatant;
(2) BCG ∆leuD/Ag85B lysate; (3) wild type BCG ∆leuD (negative control). BCG ∆leuD/Ag85B
inhibits cell proliferation of human bladder carcinoma cells after 48 h of treatment (B). Cell
proliferation was investigated by MTT assay. Data are expressed as mean ± SEM from three
independent experiments. Significance was considered at P0.05.
48
Figure 2: BCG ∆leuD/Ag85B increased 5637 cell death. Bladder cancer cells were
treated with BCG strains for 48 h. Quantitative analysis of cell death was estimated
by LIVE/DEAD assay. Untreated cells (A); BCG Pasteur treatment (B); BCG
∆leuD/Ag85B treatment (C); BCG strains alone after 48 h of co-culture with 5637 cell
line (D).
49
Figure 3: BCG ∆leuD/Ag85B treatment changes apoptotic gene expression profile in 5637
cells. Bladder cancer cell line was treated with BCG strains for 48 h. Gene expression profile
was investigated by qRT-PCR. Anti-apoptotics Bcl-2 and Survivin genes (A); Pro-apoptotic
Bax gene, AIF and Endonuclease G genes (B). Data are expressed as mean ± SEM from
three independent experiments. Different letters indicate significant differences among
means. The significance was considered at P0.05.
50
Figure 4: BCG ∆leuD/Ag85B treatment increased bax/bcl-2 ratio in 5637 cell line.
Bladder cancer cells were treated with BCG strains for 48 h. Gene expression profile
was investigated by qRT-PCR. Data are expressed as mean ± SEM from three
independent experiments. Different letters indicate significant differences among
means. The significance was considered at P0.05.
51
Figure 5: BCG ∆leuD/Ag85B treatment increased caspases gene expression in
bladder cancer cell line. 5637 cell line was treated with BCG strains for 48 h. Gene
expression profile was investigated by qRT-PCR. Caspase-3 (A); caspase-8 (B);
caspase-9 (C). Data are expressed as mean ± SEM from three independent
experiments. Different letters indicate significant differences among means. The
significance was considered at P0.05.
52
Figure 6: BCG ∆leuD/Ag85B changes antioxidant enzymes gene expression in 5637
cells. Bladder cancer cell line was treated with BCG strains for 48 h. Gene
expression profile was investigated by qRT-PCR. Cu/Zn-SOD, Mn-SOD, CAT, and
GPx (A); GST and TRX (B). Data are expressed as mean ± SEM from three
independent experiments. Different letters indicate significant differences among
means. The significance was considered at P0.05.
53
Figure 7: BCG ∆leuD/Ag85B changes p53 and p21 gene expression in bladder
cancer cells. 5637 cell line was treated with BCG strains for 48 h. Gene expression
profile was investigated by qRT-PCR. Data are expressed as mean ± SEM from
three independent experiments. Different letters indicate significant differences
among means. The significance was considered at P0.05.
54
4. CONCLUSÕES
A
cepa
auxotrófica
de
BCG
superexpressando
Ag85B
aumenta
a citotoxicidade em células de câncer superficial de bexiga em modelo in vitro,
e esse efeito pode ocorrer devido a apoptose;
BCG ∆leuD/Ag85B aumenta os níveis de mRNA de genes apoptóticos;
BCG ∆leuD/Ag85B modifica o padrão de expressão gênica de genes
relacionados ao ciclo celular;
BCG ∆leuD/Ag85B eleva os níveis de expressão de enzimas antioxidantes;
A cepa BCG ∆leuD/Ag85B pode ser um agente terapêutico mais eficaz ao
câncer de bexiga do que as cepas atualmente disponíveis para imunoterapia.
55
5. REFERÊNCIAS
ALDRICH, J.F.; LOWE, D.B.; SHEARER, M.H.; WINN, R.E.; JUMPER, C.A.;
KENNEDY, R.C. Vaccines and immunotherapeutics for the treatment of malignant
disease. Clin.Dev.Immunol., 697158, 2010.
AMIRKHAH, R.; KHANAHMAD, H.; ABOLHASSANI, M.; POOYA, M.; MOVASSAGH,
H.; SHOKRGOZAR, M.A. Improvement of bladder cancer immunotherapy by creating
a recombinant Bacille Calmette-Gu'erin which secrets p53 protein. Med.Hypotheses,
v. 72, p. 754, 2009.
AMOS, S.M.; DUONG, C.P.; WESTWOOD, J.A.; RITCHIE, D.S.; JUNGHANS, R.P.;
DARCY, P.K.; KERSHAW, M.H. Autoimmunity associated with immunotherapy of
cancer. Blood, v. 118, p. 499-509, 2011.
ANASSI, E.; NDEFO, U.A. Sipuleucel-T (provenge) injection: the first immunotherapy
agent (vaccine) for hormone-refractory prostate cancer. P.T., v. 36, p. 197-202, 2011.
ANDRADE, P.M.; CHADE, D.C.; BORRA, R.C.; NASCIMENTO, I.P.; VILLANOVA,
F.E.; LEITE, L.C.; ANDRADE, E.; SROUGI, M. The therapeutic potential of
recombinant BCG expressing the antigen S1PT in the intravesical treatment of
bladder cancer. Urol.Oncol., v. 28, p. 520-525, 2010.
BASTOS, R.G.; BORSUK, S.; SEIXAS, F.K.; DELLAGOSTIN, O.A. Recombinant
Mycobacterium bovis BCG. Vaccine, v. 27, p. 6495-6503, 2009.
BEHR, M.A.; SMALL, P.M. A historical and molecular phylogeny of BCG strains.
Vaccine, v. 17, p. 915-922, 1999.
BENEVOLO-DE-ANDRADE, T.C.; MONTEIRO-MAIA, R.; COSGROVE, C.;
CASTELLO-BRANCO, L.R. BCG Moreau Rio de Janeiro: an oral vaccine against
tuberculosis--review. Mem.Inst.Oswaldo Cruz, v. 100, p. 459-465, 2005.
BOHLE, A.; BRANDAU, S. Immune mechanisms in bacillus Calmette-Guerin
immunotherapy for superficial bladder cancer. J.Urol., v. 170, p. 964-969, 2003.
56
CHUNG, M.A.; LUO, Y.; O'DONNELL, M.; RODRIGUEZ, C.; HEBER, W.;
SHARMA, S.; CHANG, H.R. Development and preclinical evaluation of a
Bacillus Calmette-Guerin-MUC1-based novel breast cancer vaccine. Cancer
Res., v. 63, p. 1280-1287, 2003.
COE, J.E.; FELDMAN, J.D. Extracutaneous delayed hypersensitivity,
particularly in the guinea-pig bladder. Immunology, v. 10, p. 127-136, 1966.
DENIS, O.; LOZES, E.; HUYGEN, K. Induction of cytotoxic T-cell responses
against culture filtrate antigens in Mycobacterium bovis bacillus CalmetteGuerin-infected mice. Infect.Immun., v. 65, p. 676-684, 1997.
DRANOFF, G. Cytokines in cancer pathogenesis and cancer therapy.
Nat.Rev.Cancer, v. 4, p. 11-22, 2004.
GILBOA, E. The promise of cancer vaccines. Nat.Rev.Cancer, v. 4, p. 401-411,
2004.
GONTERO, P.; BOHLE, A.; MALMSTROM, P.U.; O'DONNELL, M.A.;
ODERDA, M.; SYLVESTER, R.; WITJES, F. The role of bacillus CalmetteGuerin in the treatment of non-muscle-invasive bladder cancer. Eur.Urol., v. 57,
p. 410-429, 2010.
HERR, H.W.; MORALES, A. History of bacillus Calmette-Guerin and bladder
cancer: an immunotherapy success story. J.Urol., v. 179, p. 53-56, 2008.
INCA – Estimativa 2012, Incidência de Câncer no Brasil. Disponível em
http://www.inca.gov.br/, acessado em 01/02/2012.
JACOBS Jr, W.R.; TUCKMAN, M.; BLOOM, B.R. Introduction of foreign DNA
into mycobacteria using a shuttle phasmid. Nature, v. 327, p. 532-535, 1987.
JAGANNATH, C.; LINDSEY, D.R.; DHANDAYUTHAPANI, S.; XU, Y.;
HUNTER, R.L.; EISSA, N.T. Autophagy enhances the efficacy of BCG vaccine
by increasing peptide presentation in mouse dendritic cells. Nat.Med., v. 15, p.
267-276, 2009.
JUNG, I.; MESSING, E. Molecular mechanisms and pathways in bladder cancer
development and progression. Cancer Control, v. 7, p. 325-334, 2000.
KRESOWIK, T.P.; GRIFFITH, T.S. Bacillus Calmette-Guerin immunotherapy for
urothelial carcinoma of the bladder. Immunotherapy., v. 1, p. 281-288, 2009.
LAGRANDERIE, M.R.; BALAZUC, A.M.; DERIAUD, E.; LECLERC, C.D.;
GHEORGHIU, M. Comparison of immune responses of mice immunized with
57
five different Mycobacterium bovis BCG vaccine strains. Infect.Immun., v. 64,
p. 1-9, 1996.
LAMM, D.L. Complications of bacillus Calmette-Guerin immunotherapy.
Urol.Clin.North Am., v. 19, p. 565-572, 1992.
LAMM, D.L.; THOR, D.E.; HARRIS, S.C.; REYNA, J.A.; STOGDILL, V.D.;
RADWIN, H.M. Bacillus Calmette-Guerin immunotherapy of superficial bladder
cancer. J.Urol., v. 124, p. 38-40, 1980.
LEE, C.F.; CHANG, S.Y.; HSIEH, D.S.; YU, D.S. Treatment of bladder
carcinomas using recombinant BCG DNA vaccines and electroporative gene
immunotherapy. Cancer Gene Ther., v. 11, p. 194-207, 2004.
LIN, C.W.; SU, I.J.; CHANG, J.R.; CHEN, Y.Y.; LU, J.J.; DOU, H.Y.
Recombinant BCG coexpressing Ag85B, CFP10, and interleukin-12 induces
multifunctional Th1 and memory T cells in mice. APMIS, v. 120, p. 72-82, 2012.
LIU, W.; O'DONNELL, M.A.; CHEN, X. HAN, R.; LUO, Y. Recombinant bacillus
Calmette-Guerin (BCG) expressing interferon-alpha 2B enhances human
mononuclear cell cytotoxicity against bladder cancer cell lines in vitro. Cancer
Immunol.Immunother., 58, 1647-1655, 2009.
LUDWIG, A.T.; MOORE, J.M.; LUO, Y.; CHEN, X.; SALTSGAVER, N.A.;
O'DONNELL, M.A.; GRIFFITH, T.S. Tumor necrosis factor-related apoptosisinducing ligand: a novel mechanism for Bacillus Calmette-Guerin-induced
antitumor activity. Cancer Res., v. 64, p. 3386-3390, 2004
LUO, Y.; CHEN, X.; HAN, R.; O'DONNELL, M.A. Recombinant bacille CalmetteGuerin (BCG) expressing human interferon-alpha 2B demonstrates enhanced
immunogenicity. Clin.Exp.Immunol., v. 123, p. 264-270, 2001.
LUO, Y.; CHEN, X.; O'DONNELL, M.A. Role of Th1 and Th2 cytokines in BCGinduced IFN-gamma production: cytokine promotion and simulation of BCG
effect. Cytokine, v. 21, p. 17-26, 2003.
LUO, Y.; HAN, R.; EVANOFF, D.P.; CHEN, X. Interleukin-10 inhibits
Mycobacterium bovis bacillus Calmette-Guerin (BCG)-induced macrophage
cytotoxicity against bladder cancer cells. Clin.Exp.Immunol., v. 160, p. 359368, 2010.
LUO, Y.; WANG, B.; HU, L.; YU, H.; DA, Z.; JIANG, W.; SONG, N.; QIE, Y.;
WANG, H.; TANG, Z.; XIAN, Q.; ZHANG, Y.; ZHU, B. Fusion protein Ag85BMPT64(190-198)-Mtb8.4 has higher immunogenicity than Ag85B with capacity
58
to boost BCG-primed immunity against Mycobacterium tuberculosis in mice.
Vaccine, v. 27, p. 6179-6185, 2009.
LUO, Y.; YAMADA, H.; CHEN, X.; RYAN, A.A.; EVANOFF, D.P.; TRICCAS,
J.A.; O'DONNELL, M.A. Recombinant Mycobacterium bovis bacillus CalmetteGuerin (BCG) expressing mouse IL-18 augments Th1 immunity and
macrophage cytotoxicity. Clin.Exp.Immunol., v. 137, p. 24-34, 2004.
LUO, Y.; YAMADA, H.; EVANOFF, D.P.; CHEN, X. Role of Th1-stimulating
cytokines in bacillus Calmette-Guerin (BCG)-induced macrophage cytotoxicity
against mouse bladder cancer MBT-2 cells. Clin.Exp.Immunol., v. 146, p. 181188, 2006.
MADAN, R.A.; MOHEBTASH, M.; SCHLOM, J.; GULLEY, J.L. Therapeutic
vaccines in metastatic castration-resistant prostate cancer: principles in clinical
trial design. Expert.Opin.Biol.Ther., v. 10, p. 19-28, 2010.
MATHE, G.; CATTAN, A.; AMIEL, J.L.; SCHWARZENBERG, L.; SCHNEIDER,
M. Experimental therapeutic trials of leukemia and hematosarcomas:
technologic and philosophic aspects. Ann.N.Y.Acad.Sci., 164, 776-792, 1969.
MATSUO, K.; YAMAGUCHI, R.; YAMAZAKI, A.; TASAKA, H.; TERASAKA, K.;
TOTSUKA, M.; KOBAYASHI, K.; YUKITAKE, H.; YAMADA, T. Establishment of
a foreign antigen secretion system in mycobacteria. Infect.Immun., 58, 40494054, 1990.
MINNIKIN, D.E.; PARLETT, J.H.; MAGNUSSON, M.; RIDELL, M.; LIND, A.
Mycolic acid patterns of representatives of Mycobacterium bovis BCG.
J.Gen.Microbiol., v. 130, p. 2733-2736, 1984.
MORALES, A.; EIDINGER, D.; BRUCE, A.W. Intracavitary Bacillus CalmetteGuerin in the treatment of superficial bladder tumors. J.Urol., v. 116, p. 180183, 1976.
MUSTAFA, A.S.; AMOUDY, H.A.; WIKER, H.G.; ABAL, A.T.; RAVN, P.;
OFTUNG, F.; ANDERSEN, P. Comparison of antigen-specific T-cell responses
of tuberculosis patients using complex or single antigens of Mycobacterium
tuberculosis. Scand.J.Immunol., v. 48, p. 535-543, 1998.
NAITO, M.; OHARA, N.; MATSUMOTO, S.; YAMADA, T. The novel fibronectinbinding motif and key residues of mycobacteria. J.Biol.Chem., v. 273, p. 29052909, 1998.
59
NEPPLE, K.G.; AUBERT, H.A.; BRAASCH, M.R.; O'DONNELL, M.A.
Combination of BCG and interferon intravesical immunotherapy: an update.
World J.Urol., v. 27, p. 343-346, 2009.
O'DONNELL, M.A. The genetic reconstruction of BCG as a
immunotherapeutic tool. Trends Biotechnol., v. 15, p. 512-517, 1997.
new
OHARA, N.; YAMADA, T. Recombinant BCG vaccines. Vaccine, v. 19, p. 40894098, 2001.
OLD, L.J.; CLARKE, D.A.; BENACERRAF, B. Effect of Bacillus CalmetteGuerin infection on transplanted tumours in the mouse. Nature, v. 184(Suppl 5),
p. 291-292, 1959.
PASHOS, C.L.; BOTTEMAN, M.F.; LASKIN, B.L.; REDAELLI, A. Bladder
cancer: epidemiology, diagnosis, and management. Cancer Pract., v. 10, p.
311-322, 2002.
PEARL, R. Cancer and tuberculosis. Am J Hygiene, v. 9, p. 97-102, 1929.
SCHENK-BRAAT, E.A.; BANGMA, C.H. Immunotherapy for superficial bladder
cancer. Cancer Immunol.Immunother., v. 54, p. 414-423, 2005.
SCHREIBER, R.D.; OLD, L.J.; SMYTH, M.J. Cancer immunoediting: integrating
immunity's roles in cancer suppression and promotion. Science, v. 331, p.
1565-1570, 2011.
SHENG, W.Y.; HUANG, L. Cancer immunotherapy and nanomedicine.
Pharm.Res., v. 28, p. 200-214, 2011.
SIEGEL, R.; WARD, E.; BRAWLEY, O.; JEMAL,A. Cancer statistics, 2011: the
impact of eliminating socioeconomic and racial disparities on premature cancer
deaths. CA Cancer J.Clin., v. 61, p. 212-236, 2011.
SIMONS, M.P.; NAUSEEF, W.M.; GRIFFITH, T.S. Neutrophils and TRAIL:
insights into BCG immunotherapy for bladder cancer. Immunol.Res., v. 39, p.
79-93, 2007.
SNAPPER, S.B.; LUGOSI, L.; JEKKEL, A.; MELTON, R.E.; KIESER, T.;
BLOOM, B.R.; JACOBS Jr, W.R. Lysogeny and transformation in mycobacteria:
stable expression of foreign genes. Proc.Natl.Acad.Sci.U.S.A, v. 85, p. 69876991, 1988.
SUTTMANN, H.; RIEMENSBERGER, J.; BENTIEN, G.; SCHMALTZ, D.;
STOCKLE, M.; JOCHAM, D.; BOHLE, A.; BRANDAU, S. Neutrophil
granulocytes are required for effective Bacillus Calmette-Guerin immunotherapy
60
of bladder cancer and orchestrate local immune responses. Cancer Res., v. 66,
p. 8250-8257, 2006.
SYLVESTER, R.J.; VAN DER MEIJDEN, A.; WITJES, J.A.; JAKSE, G.;
NONOMURA, N.; CHENG, C.; TORRES, A.; WATSON, R.; KURTH, K.H. Highgrade Ta urothelial carcinoma and carcinoma in situ of the bladder. Urology, v.
66, p. 90-107, 2005.
SYLVESTER, R.J.; VAN DER MEIJDEN, A.P.; LAMM, D.L. Intravesical bacillus
Calmette-Guerin reduces the risk of progression in patients with superficial
bladder cancer: a meta-analysis of the published results of randomized clinical
trials. J.Urol., v. 168, p. 1964-1970, 2002.
THALMANN, G.N.; SERMIER, A.; RENTSCH, C.; MOHRLE, K.; CECCHINI,
M.G.; STUDER, U.E. Urinary Interleukin-8 and 18 predict the response of
superficial bladder cancer to intravesical therapy with bacillus Calmette-Guerin.
J.Urol., v. 164, p. 2129-2133, 2000.
TRICCAS, J.A. Recombinant BCG as a vaccine vehicle to protect against
tuberculosis. Bioeng.Bugs., 1, 110-115, 2010.
WIKER, H.G.; HARBOE, M. The antigen 85 complex: a major secretion product
of Mycobacterium tuberculosis. Microbiol.Rev., v. 56, p. 648-661, 1992.
WU, X.R. Urothelial tumorigenesis:
Nat.Rev.Cancer, v. 5, p. 713-725, 2005.
a
tale
of
divergent
pathways.
ZBAR, B.; TANAKA, T. Immunotherapy of cancer: regression of tumors after
intralesional injection of living Mycobacterium bovis. Science, 172, 271-273,
1971.
ZEEGERS, M.P.; TAN, F.E.; DORANT, E.; VAN DEN BRANDT, P.A. The
impact of characteristics of cigarette smoking on urinary tract cancer risk: a
meta analysis of epidemiologic studies. Cancer, v. 89, p. 630-639, 2000.
ZHENG, Y.; IZUMI, K.; YAO, J.L.; MIYAMOTO,H. Dihydrotestosterone
upregulates the expression of epidermal growth factor receptor and ERBB2 in
androgen receptor-positive bladder cancer cells. Endocr.Relat Cancer,