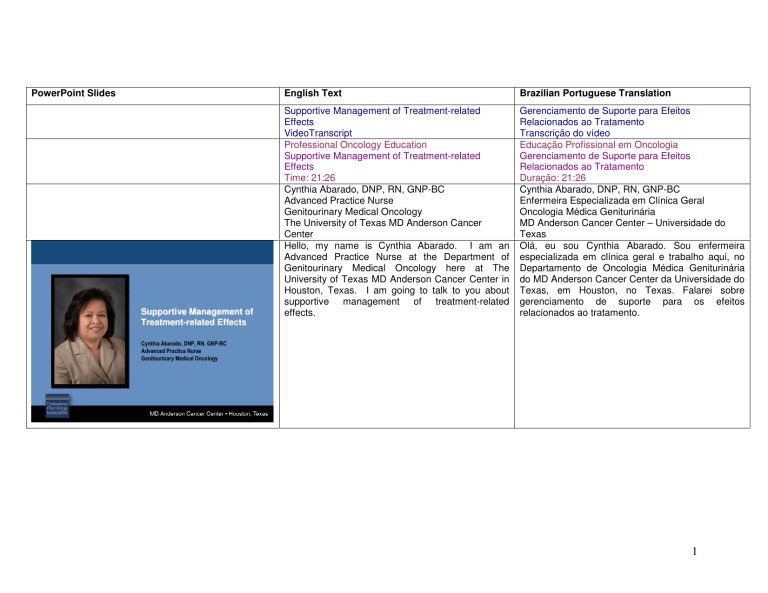
PowerPoint Slides
Supportive Management of
TreatmentTreatment-related Effects
Supportive Management of
TreatmentTreatment-related Effects
English Text
Brazilian Portuguese Translation
Supportive Management of Treatment-related
Effects
VideoTranscript
Professional Oncology Education
Supportive Management of Treatment-related
Effects
Time: 21:26
Cynthia Abarado, DNP, RN, GNP-BC
Advanced Practice Nurse
Genitourinary Medical Oncology
The University of Texas MD Anderson Cancer
Center
Hello, my name is Cynthia Abarado. I am an
Advanced Practice Nurse at the Department of
Genitourinary Medical Oncology here at The
University of Texas MD Anderson Cancer Center in
Houston, Texas. I am going to talk to you about
supportive management of treatment-related
effects.
Gerenciamento de Suporte para Efeitos
Relacionados ao Tratamento
Transcrição do vídeo
Educação Profissional em Oncologia
Gerenciamento de Suporte para Efeitos
Relacionados ao Tratamento
Duração: 21:26
Cynthia Abarado, DNP, RN, GNP-BC
Enfermeira Especializada em Clínica Geral
Oncologia Médica Geniturinária
MD Anderson Cancer Center – Universidade do
Texas
Olá, eu sou Cynthia Abarado. Sou enfermeira
especializada em clínica geral e trabalho aqui, no
Departamento de Oncologia Médica Geniturinária
do MD Anderson Cancer Center da Universidade do
Texas, em Houston, no Texas. Falarei sobre
gerenciamento de suporte para os efeitos
relacionados ao tratamento.
Cynthia Abarado, DNP, RN, GNP-BC
Advanced Practice Nurse
Genitourinary Medical Oncology
1
Supportive Management of
TreatmentTreatment-related Effects
Objectives
Upon completion of this lesson, participants will
be able to:
Objectives of this presentation are as follows: to
identify
common
treatment-related
effects,
recognize signs and symptoms of these conditions,
and identify management options to minimize these
effects.
Os objetivos da apresentação são: identificar os
efeitos comuns relacionados ao tratamento,
reconhecer os sinais e sintomas destas doenças e
identificar as opções de gerenciamento para
minimizar tais efeitos.
Anemia is one of the most common cancer
treatment-related effects. Anemia is defined as a
hemoglobin less than 11 g/dl. Some causes of
anemia [are] related to blood loss, hemolysis,
suppression of erythropoiesis and erythropoietin
products by inflammatory cytokines, chemotherapy,
radiation, nutritional deficiencies, as well as renal
impairment.
A anemia é um dos efeitos mais comuns
relacionados ao tratamento antineoplásico. Definese a anemia como uma concentração de
hemoglobina inferior a 11 g/dl. Algumas causas de
anemia [estão] relacionadas à perda de sangue,
hemólise, supressão da eritropoiese e produtos de
eritropoietina
pelas
citocinas
inflamatórias,
quimioterapia, radiação, deficiências nutricionais e
insuficiência renal.
• Identify common treatment-related effects
• Recognize signs and symptoms of these conditions
• Identify management options to minimize
these effects
Supportive Management of
TreatmentTreatment-related Effects
Anemia
• Anemia is defined as a hemoglobin less than
11 g/dl.
• Causes of anemia:
– Blood loss
– Hemolysis
– Suppression of erythropoiesis and erythropoietin
products by inflammatory cytokines
– Chemotherapy
– Radiation
– Nutritional deficiencies
– Renal impairment
NCCN GuidelinesTM, 2007, www.nccn.org
2
Supportive Management of
TreatmentTreatment-related Effects
Manifestations of Anemia
Some of the manifestations of anemia are fatigue,
dizziness, vertigo, depression, impaired cognitive
function, anorexia, nausea, pallor, low skin
temperature.
Algumas das manifestações de anemia são: fadiga,
tontura, vertigem, depressão, comprometimento da
função cognitiva, anorexia, náuseas, palidez e baixa
temperatura da pele.
Impaired T-cell and macrophage function, exertional
dyspnea, tachycardia, palpitations, increased pulse
pressure, risk of life-threatening cardiac failure, as
well as menstrual problems and loss of libido.
Comprometimento da função de células T e
macrófagos, dispneia de esforço, taquicardia,
palpitações, aumento da pressão arterial de pulso,
risco de insuficiência cardíaca com risco de vida,
bem como problemas menstruais e perda de libido.
• CNS
–
–
–
–
Fatigue
Dizziness, vertigo
Depression
Impaired cognitive function
• GI System
– Anorexia
– Nausea
• Vascular System
– Pallor
– Low skin temperature
Supportive Management of
TreatmentTreatment-related Effects
Manifestations of Anemia
• Immune System
– Impaired t-cell and macrophage function
• Cardiovascular system
–
–
–
–
Exertional dyspnea
Tachycardia, palpitations
Increased pulse pressure
Risk of life-threatening cardiac failure
• Genital Tract
– Menstrual problems
– Loss of libido
3
Supportive Management of
TreatmentTreatment-related Effects
Laboratory Assessment of Anemia
• Hemoglobin – the amount of hemoglobin or
the oxygen capacity of the peripheral blood
• Hematocrit – the space or volume occupied
by the red cells in relation to the blood volume
Some of the laboratory assessment of anemia
include measurements of hemoglobin, which is the
amount of oxygen capacity of the peripheral blood;
hematocrit, which is the space or volume occupied
by the red cells in relation to the blood volume; MCV
or mean corpuscular volume, which is the average
volume or size of a single RBC in a given blood
sample.
Algumas das avaliações laboratoriais de anemia
compreendem: medições de hemoglobina, que é a
quantidade ou capacidade de oxigênio do sangue
periférico; hematócrito, que é o espaço ou volume
ocupado pelas hemácias em relação ao volume
sanguíneo; VGM ou volume globular médio, que é o
volume ou tamanho médio de uma única hemácia
em uma determinada amostra de sangue.
Other measurements are MCH, or the mean
corpuscular hemoglobin or the average weight of
hemoglobin in each RBC; the MCHC, which is the
average hemoglobin concentration or color of the
red blood cell; RDW, which is an automated
calculation of variation in size providing the
homogeneity or heterogeneity of the red cell
distribution width.
Outras medições são a HGM, ou hemoglobina
globular média ou o peso médio da hemoglobina
em cada hemácia; CHGM, que é a concentração
média de hemoglobina globular ou cor da hemácia;
RDW, que é um cálculo automatizado da variação
do tamanho, dependendo da homogeneidade ou
heterogeneidade da amplitude de distribuição das
hemácias.
• MCV – (mean corpuscular volume) the
average volume or size of a single RBC
in a given blood sample
Supportive Management of
TreatmentTreatment-related Effects
Laboratory Assessment of Anemia
• MCH – (mean corpuscular hemoglobin) the average
weight of hemoglobin in each RBC
• MCHC – (mean corpuscular hemoglobin
concentration) the average hemoglobin
concentration or color of the RBC
• RDW – (red cell distribution width) an automated
calculation of variation in size, which provides
homogeneity (normal RDW) or heterogeneity (high
RDW)
4
Supportive Management of
TreatmentTreatment-related Effects
Assessment of Types of Anemias
Some other assessments for different types of
anemias include measurement of the reticulocyte
count, ferritin, transferrin, serum iron, Coombs test,
serum B12, and folate levels.
Outras avaliação para diferentes tipos de anemias
incluem a medição da contagem de reticulócitos,
ferritina, transferrina, ferro sérico, teste de Coombs,
níveis de [vitamina] B12 e folato no soro.
Some of the strategies in treatment of anemia
include parenteral iron administration, blood
transfusion, as well as administration of the
erythropoiesis-stimulating factors. Indications for
the erythropoiesis-stimulating factors have side
effects and these include: interruption or
modification based on hemoglobin levels of patients,
reports [of] increased mortality, and thrombotic
vascular events. So patients have to be monitored
for a risk of pulmonary embolism, DVT, and edema.
Algumas estratégias no tratamento da anemia são:
administração parenteral de ferro, transfusão de
sangue, bem como a administração de fatores
estimulantes da eritropoiese. [Pacientes que
recebem] fatores estimulantes da eritropoiese
apresentam efeitos colaterais, dentre os quais:
interrupção ou modificação com base nos níveis de
hemoglobina dos pacientes, relatos [de] aumento
da mortalidade e eventos vasculares trombóticos.
Assim, os pacientes devem ser monitorados quanto
ao risco de embolia pulmonar, trombose venosa
profunda e edema.
• Reticulocyte count
• Ferritin
• Transferrin
• Serum iron
• Coomb’s test
• Serum B12 and folate levels
Supportive Management of
TreatmentTreatment-related Effects
Treatment of Anemia
• Parenteral iron administration
• Blood transfusion
• Erythropoiesis-stimulating-epoetin, darbepoetin
- Indications/side effects
• Interruption or modification based on hemoglobin
levels of patients; reports increased mortality and
thrombotic vascular events
• Adverse reactions including pure red cell aplasia,
pulmonary embolism, DVT and edema
5
Supportive Management of
TreatmentTreatment-related Effects
Impact of Anemia
• Quality of life
• Significant effects on therapeutic outcomes
How does anemia affect an individual? It can affect
the patient’s quality of life. It has significant effects
on therapeutic outcomes. It has also an impact on
the patient’s physical functioning and performance
status, as well as psychosocial effects. It affects the
prognosis and overall survival as well.
Como a anemia afeta a pessoa? Pode afetar a
qualidade de vida do paciente. Produz efeitos
significativos nos resultados terapêuticos. Além
disso, exerce um impacto na condição do
funcionamento e do desempenho físicos do
paciente, bem como efeitos psicossociais. Também
afeta o prognóstico e a sobrevida global.
The other cancer treatment-related effect is
neutropenia. It is diagnosed by absolute neutrophil
count. Absolute neutrophil count of less than 2,000
is neutropenia. The patient’s normal range of the
3
ANC is around 2,500-6,000/mm of blood or primary
white cell. ANC of less than 500 places a patient at
severe risk for infection. Nadir is the time when the
white cell counts are at their lowest point. Typically,
it occurs at around 10 to 14 days after
chemotherapy and requires 3 to 4 weeks for
recovery.
O outro efeito relacionado ao tratamento
antineoplásico é a neutropenia. É diagnosticada
pela contagem absoluta de neutrófilos [CAN]. Uma
contagem absoluta de neutrófilos abaixo de 2.000 é
considerada neutropenia. A faixa normal de CAN
3
nos pacientes varia de 2.500 a 6.000/mm de
sangue ou leucócitos primários. A CAN inferior a
500 expõe o paciente a graves riscos de infecções.
Nadir é o tempo em que a contagem de leucócitos
atinge a mínima concentração. Normalmente,
ocorre de 10 a 14 dias após a quimioterapia e
requer de 3 a 4 semanas para o restabelecimento.
• Physical impact
• Psychosocial impact
• Prognosis and survival
Supportive Management of
TreatmentTreatment-related Effects
Neutropenia
• Diagnosed by absolute neutrophil count (ANC)
– Normal range 2,500 - 6,000 per cubic
millimeter of blood (primary white cell)
– ANC < 2,000 = neutropenia
– ANC < 500 places a patient at severe
risk for infection
– Nadir
• Time when WBCs are at their lowest point
• Typically 10 to 14 days after chemotherapy
• Recovery may take 3 to 4 weeks
6
Supportive Management of
TreatmentTreatment-related Effects
Neutropenic Infection
• Symptoms/signs
–
–
–
–
–
–
–
Fever greater than 100.4°F (38°C)
Chills/sweating
Sore throat or cough
Mouth ulcers
Diarrhea
Burning sensation during urination
Redness, pain, or swelling around a wound or sore
Supportive Management of
TreatmentTreatment-related Effects
Management of Neutropenia
• Prophylactic use of growth factors, when indicated:
pegfilgrastim, filgrastim
• Good hand-washing technique
• Early detection and treatment of infection
• Follow treatment guidelines to reduce mortality
If the patient is neutropenic, he is at risk for
developing infection. And some of the signs and
symptoms of infection are temperature of greater
°
than 38 C or 100.4°F, chills, sweating, sore throat,
mouth ulcers, diarrhea, burning sensation during
urination, or redness, pain, or swelling around a
wound or sore.
Pacientes neutropênicos estão em risco de adquirir
infecções. E alguns dos sinais e sintomas de
°
infecção são: temperaturas acima de 38 C ou 100,4
°F, calafrios, suores, dor de garganta, ulcerações
na boca, sensação de ardência ao urinar ou
eritema, dor ou inchaço ao redor de ferida ou
chaga.
How do we manage neutropenia?
After
chemotherapy, a prophylactic use of growth factors
when indicated, such as Neupogen or Neulasta,
is recommended. The best prevention for infection
is a good hand washing technique. Also early
detection and treatment of infection can have
positive outcome and prevent sepsis or infection.
TM
The NCCN Guidelines
recommend following
treatment guidelines to reduce mortality in the
management of neutropenia.
Como controlamos a neutropenia? Quando
indicado, recomenda-se o uso profilático de fatores
de crescimento, como Neupogen ou Neulasta
depois da quimioterapia. A melhor prevenção contra
infecção é uma boa técnica para lavar as mãos.
Além disso, detecção e tratamento precoces da
infecção podem trazer resultados positivos e evitar
TM
sepse ou infecção. As NCCN Guidelines
recomendam
as
seguintes
diretrizes
para
tratamento com o objetivo de reduzir a mortalidade
no manejo da neutropenia.
NCCN GuidelinesTM, 2007, www.nccn.org
7
Supportive Management of
TreatmentTreatment-related Effects
Treatment-related Nutritional Effects
• Chemotherapy and radiation therapy
–
–
–
–
–
–
–
–
Weight loss
Fatigue
Nausea/vomiting
Taste alterations
Oral mucositis
Constipation (chemo only)
Xerostomia
Anorexia
Supportive Management of
TreatmentTreatment-related Effects
Treatment-related Nutritional Side-effects
• Surgery
–
–
–
–
–
Other treatment-related side effects are very
significant in the nutritional effects of chemotherapy
and nutrition and some of these are manifested as
in weight loss, fatigue, nausea, vomiting, taste
alterations, oral mucositis, constipation (only in
chemotherapy though because radiation would have
more of a diarrhea side effect), xerostomia, and
anorexia.
Outros efeitos colaterais relacionados ao tratamento
são muito significativos nos efeitos nutricionais da
quimioterapia e da nutrição e alguns deles se
manifestam como emagrecimento, fadiga, náusea,
vômito, alteração do paladar, mucosite oral,
constipação (somente na quimioterapia, porque a
radiação produziria um efeito colateral do tipo
diarreia), xerostomia e anorexia.
Specifically surgery can also cause weight loss,
fatigue, nausea, vomiting, diarrhea, and loss of
appetite. Immunotherapy again can cause weight
loss, fatigue, oral mucositis, diarrhea, as well as
anorexia.
Especificamente, a cirurgia também pode causar
emagrecimento, fadiga, náusea, vômito, diarreia e
perda de apetite. A imunoterapia também pode
causar emagrecimento, fadiga, mucosite oral,
diarreia e anorexia.
Weight loss
Fatigue
Nausea/vomiting
Diarrhea
Loss of appetite
• Immunotherapy
–
–
–
–
–
Weight loss
Fatigue
Oral mucositis
Diarrhea
Anorexia
8
Supportive Management of
TreatmentTreatment-related Effects
Oral Mucositis
• Most common complication associated
with chemotherapy
• Affects 40% of individuals on chemotherapy
– 80% of individuals receiving bone
marrow transplant
– 100% of individuals receiving head
and neck radiation
Supportive Management of
TreatmentTreatment-related Effects
Mucositis
• Mucosal injury characterized by ulceration in
the oro-esophageal and gastrointestinal mucosa
The most devastating treatment-related side effect,
in terms of the digestive tract, is a development of
oral mucositis, which is the most common
complication
associated
with
chemotherapy.
Around 40% of individuals on chemotherapy
develop mucositis, 80% of individuals receiving
bone marrow transplant and 100% of individuals
receiving head and neck radiation would develop
oral mucositis.
O pior efeito colateral relacionado ao tratamento em
termos de trato digestivo é a mucosite oral, que é a
complicação
mais
comum
associada
à
quimioterapia. Cerca de 40% das pessoas que
recebem quimioterapia apresentam mucosite, 80%
das pessoas que recebem transplante de medula
óssea e 100% de pessoas que recebem radiação
na cabeça e pescoço apresentariam mucosite oral.
So, what is mucositis? It is a mucosal injury
characterized by ulceration in the oral esophageal
and gastrointestinal mucosa. Some of the effects
from mucositis are related to pain, dysphagia,
diarrhea, dehydration and also it poses as the
greatest risk for bacteremia and sepsis.
Então, o que é mucosite? É uma lesão da mucosa
caracterizada por ulceração na mucosa oral,
esofágica e gastrointestinal. Alguns dos efeitos da
mucosite estão relacionados à dor, disfagia,
diarreia, desidratação e também representa o maior
risco para bacteremia e sepse.
• Effects:
–
–
–
–
Pain
Dysphagia
Diarrhea
Dehydration
• Risk factor for bacteremia and sepsis
9
Supportive Management of
TreatmentTreatment-related Effects
Pathogenesis: Oral Mucositis
1) Initiation: DNA and non-DNA damage, direct cellular
injury to basal epithelial cells, generation of reactive
oxygen species
2) Primary damage response: Damage in genes is
followed by upregulation of genes, which results in
the production of a range of destructive proteins and
molecules such as the proinflammatory cytokines
that lead to apoptosis and tissue injury
How does oral mucositis develop? There are
several phases that occur. And with the introduction
of the chemotherapy and radiation the first stage is
the initiation where DNA and non-DNA damage
direct cellular injury to basal epithelial cells and
generation of reactive oxygen species occur. A
second phase is the primary damage response.
Damage in the genes is followed by upregulation of
genes, which results in the production of a range of
destructive proteins and molecules such as the
proinflammatory cytokines that lead to tissue injury.
Como se manifesta a mucosite? Ocorrem várias
fases. Com a introdução da quimioterapia e da
radiação, a primeira fase é o início em que lesões
de DNA e não DNA direcionam a lesão celular às
células epiteliais basais, ocorrendo geração de
espécies reativas de oxigênio. A segunda fase é a
resposta ao dano primário. A lesão ocorrida nos
genes é seguida pela suprarregulação de genes,
que resulta na produção de uma série de proteínas
e moléculas destrutivas, como citocinas próinflamatórias que causam lesões nos tecidos.
The third phase is a signal amplification, where
substances from the damage response phase
provide a positive feedback loop that drives the
destructive process forward resulting to ulceration.
The oral epithelium breaks down and ulcerates. At
this point, infection can occur at any stage of this
phase, frequently corresponding to the stage of
neutropenia, and mostly it is associated with an
increase in gram-negative organisms. The fifth
phase is the healing phase, which is the biologically
dynamic phase with signaling from the submucosal
extracellular matrix stimulating the migration,
differentiation, and proliferation of the healing
epithelium.
A terceira fase é a amplificação do sinal, em que
substâncias da fase de resposta à lesão agem
como um retorno positivo que estimula o processo
destrutivo, resultando em ulceração. O epitélio oral
se rompe e forma úlceras. Neste momento, a
infecção pode ocorrer em qualquer estágio desta
fase, correspondendo frequentemente ao estágio
de neutropenia, sendo associada, sobretudo, ao
aumento de organismos gram-negativos. A quinta
fase é a de cicatrização, que é a fase
biologicamente dinâmica, com sinalização da matriz
submucosa extracelular que estimula a migração,
diferenciação e proliferação do epitélio de
cicatrização.
Scully C et al. Oral Dis 2006 12(3):229
Supportive Management of
TreatmentTreatment-related Effects
Pathogenesis: Oral Mucositis
3) Signal amplification: Substances from the damage
response phase provide a positive feedback loop that
drives the destructive process forward
4) Ulceration: The oral epithelium breaks down and
ulcerates. Infections may occur at this stage as it
frequently corresponds with neutropenia and an
increase in gram-negative organisms
5) Healing: biologically dynamic phase with signaling
from the submucosal extracellular matrix, stimulating
the migration, differentiation, and proliferation of the
healing epithelium
Scully C et al. Oral Dis 2006 12(3):229
10
Supportive Management of
TreatmentTreatment-related Effects
Phases of Mucositis
This is just a summary or an illustration of the
different phases of mucositis. Phase 1 which is the
DNA initiation, and then phase 2 is the signaling,
phase 3 is the amplification of the response, and
phase 4 is the ulceration, and phase 5 is the healing
stage.
Isto é só um resumo ou uma ilustração das
diferentes fases da mucosite. A fase 1, que
corresponde à iniciação do DNA e, depois, a fase 2
é a sinalização, a fase 3 é a amplificação da
resposta, a fase 4 é a ulceração e a fase 5 é o
estágio de cicatrização.
The incidence of oral mucositis in cancer patients
with grade 3 to 4 is very significant. Among patients
receiving radiation for head and neck, the incidence
is 85 to 100%. Among patients receiving small or
stem cell transplantation, it affects 75 to 100%, and
for solid tumor with myelosuppression, 5 to 40%.
A incidência de mucosite oral em pacientes com
câncer de grau 3 a grau 4 é muito significativa.
Entre os pacientes que recebem irradiação na
cabeça e no pescoço, a incidência é de 85% a
100%. Entre os pacientes que recebem transplante
de células pequenas ou progenitoras, afeta de 75%
a 100%, e [os portadores de] tumores sólidos com
mielossupressão, de 5% a 40%.
Adapted from Sonis ST. Nat Rev Cancer 2004 4(4):227
Supportive Management of
TreatmentTreatment-related Effects
Oral Mucositis
• Incidence among cancer patients with grade
3-4 mucositis
– Radiation for head and neck – 85-100%
– Stem cell-transplantation – 75-100%
– Solid tumors with myelosuppression – 5-40%
11
Supportive Management of
TreatmentTreatment-related Effects
Effect of Oral Mucositis on Nutrition
• Decreased dietary intake because of taste
changes, dry mouth and or pain
What are the effects of oral mucositis on nutrition?
It can cause malnutrition. It can cause a lot of
dietary decrease because of the taste changes, dry
mouth, and pain. It can also cause weight loss and
dehydration.
Quais são os efeitos da mucosite oral na nutrição?
Pode causar má nutrição. Pode causar uma grande
diminuição da dieta decorrente da alteração do
paladar, ressecamento da boca e dor. Além disso,
pode causar emagrecimento e desidratação.
The NCCN or --- correction, the National Cancer
Institute Toxicity Criteria classifies toxicity into 0 to
4. Zero, none, 1 is the erythema of the mucosa, 2 is
the patchy ulcerations or pseudomembranes, 3 is
the confluent ulcerations of pseudomembranes with
bleeding and minor trauma, and 4 is the tissue
necrosis, significant spontaneous bleeding, which
can have life-threatening consequences.
Os NCCN ou... correção, os National Cancer
Institute Toxicity Criteria classificam a toxicidade de
0 a 4. Zero, nenhuma, 1 é o eritema da mucosa, 2
são ulcerações irregulares ou pseudomembranas, 3
são ulcerações confluentes ou pseudomembranas
com hemorragias e traumas secundários e 4 é a
necrose do tecido, hemorragia espontânea
significativa, que pode ter consequências fatais.
• Malnutrition
• Weight loss
• Dehydration
Supportive Management of
TreatmentTreatment-related Effects
Toxicity Criteria of Oral Mucositis
• NCI toxicity criteria (version 2.0)
–
–
–
–
0 = none
1 = erythema of the mucosa
2 = patchy ulcerations or pseudomembranes
3 = confluent ulcerations or pseudomembranes,
bleeding with minor trauma
– 4 = tissue necrosis, significant spontaneous bleeding,
life-threatening consequences
www.cancer.gov
12
Supportive Management of
TreatmentTreatment-related Effects
Oral Examination
• Examination of:
–
–
–
–
Buccal mucosa
Soft and hard palate
Dorsum and border of tongue
Floor of mouth
Assessment of the oral mucosa is very important
when managing mucositis. Examination should
involve examination or assessment of the buccal
mucosa, soft and hard palate, the dorsum and
border of the tongue as well as the floor of the
tongue, assessed for erythema, ulcerations,
pseudomembranes, bleeding, ability to eat, pain,
and difficulty in swallowing.
É muito importante avaliar a mucosa oral quando do
manejo da mucosite. O exame deve incluir o exame
ou a avaliação da mucosa bucal, palato mole e
duro, dorso, laterais e assoalho da língua, avaliar
para eritema, ulcerações, pseudomembranas,
sangramento, capacidade de ingestão, dor e
dificuldade para deglutir.
How do we manage mucositis?
A proactive
prevention program is the best treatment. Oral care
with salt and soda mouthwashes is recommended.
Also, avoidance of caffeine, alcohol and tobacco,
avoidance of food that could irritate the mouth as
well as promotion of good oral hygiene are some of
the strategies.
Como controlamos a mucosite? O melhor
tratamento é um programa de prevenção pró-ativo.
Recomendam-se bochechos de sal e bicarbonato
de sódio para o cuidado bucal. Além disso, evitar
cafeína, álcool e tabaco, bem como alimentos que
possam irritar a boca, além de promover uma boa
higiene oral são algumas das estratégias [a seguir].
• Assess for:
–
–
–
–
–
–
–
Erythema
Ulceration
Pseudomembranes
Bleeding
Ability to eat
Pain
Difficulty swallowing
Supportive Management of
TreatmentTreatment-related Effects
Management of Mucositis
• Oral care with salt and soda mouthwashes
• Avoid caffeine, alcohol and tobacco
• Avoid foods that could irritate the mouth
• Promote good oral hygiene
13
Supportive Management of
TreatmentTreatment-related Effects
Oral Care
For oral care again good oral hygiene is
recommended. Some have used cryotherapy and
the Multinational Association of Supportive Care has
an oral care protocol which can be referred to.
Repetindo, para o cuidado bucal, recomenda-se
uma boa higiene oral. Algumas pessoas usaram
crioterapia e a Multinational Association of
Supportive Care elaborou um protocolo de cuidado
que pode ser utilizado como referência.
Oral mucositis again is the most common
complication associated with chemotherapy. Again,
it affects 40% of individuals on chemotherapy, 80%
with those with bone marrow transplant, and 100%
with head and neck radiation.
Novamente, a mucosite oral é a complicação mais
comum associada à quimioterapia. Afeta 40% de
pessoas que recebem quimioterapia, 80% naqueles
com transplante de medula óssea e 100% com
irradiação de cabeça e pescoço.
• Good oral hygiene
• Cryotherapy
• Oral care protocol
– Multinational Association of Supportive Care in
Cancer
Supportive Management of
TreatmentTreatment-related Effects
Oral Mucositis
• Most common complication associated
with chemotherapy
• Affects 40% of individuals on chemotherapy
– 80% of individuals receiving bone marrow transplant
– 100% of individuals receiving head and neck radiation
14
Supportive Management of
TreatmentTreatment-related Effects
Effect of Oral Mucositis on Nutrition
As we have mentioned, it has a lot of side effects,
which can lead to malnutrition, weight loss, and
dehydration.
Como já mencionamos, apresenta muitos efeitos
colaterais,
pode
levar
a
má
nutrição,
emagrecimento e desidratação.
We have gone through different strategies.
Já passamos por diferentes estratégias.
• Decreased dietary intake because of taste
changes, dry mouth and or pain
• Malnutrition
• Weight loss
• Dehydration
Supportive Management of
TreatmentTreatment-related Effects
Strategies
• Oral care with salt and soda mouthwashes
• Avoid caffeine, alcohol and tobacco
• Avoid foods that could irritate the mouth
• Promote good oral hygiene
15
Supportive Management of
TreatmentTreatment-related Effects
Taste Alterations
• Common among cancer patients receiving
chemotherapy and among those with head
and neck radiation
Now, we will go to the taste alterations related to
oral mucositis. Taste alterations affect 35 to 70% of
cancer patients. And the major types of taste
alterations include hypogeusia, or reduction in taste
sensitivity, ageusia, which is an absence of taste
sensation, and dysgeusia, which is the distortion of
normal taste.
Agora, abordaremos as alterações do paladar
relacionadas à mucosite oral. As alterações do
paladar afetam de 35% a 70% dos pacientes com
câncer. E os principais tipos de alterações do
paladar incluem hipogeusia, ou redução na
sensibilidade do paladar, ageusia, que é a ausência
do sentido do paladar e disgeusia, que é a distorção
do paladar normal.
So, what are the causes of taste alterations? It has
damaged taste buds. Dry mouth can lead to taste
alterations, again oral mucosa infection as well as
dental problems. Taste alterations can also be
caused by chemotherapy side effects, often
described by patients as peculiar metallic taste.
Então, quais são as causas das alterações do
paladar? Lesões nas papilas gustativas. O
ressecamento da boca pode originar alterações no
paladar, infecções da mucosa oral, bem como
problemas dentais. As alterações no paladar
também podem ser causadas pelos efeitos
secundários da quimioterapia, frequentemente
descritos pelos pacientes como um gosto metálico
peculiar.
• Affects 35% - 70% of cancer patients
• Types include:
– Hypogeusia (most common) – reduction in
taste sensitivity
– Ageusia – an absence of taste sensations
– Dysgeusia – distortion of normal taste
Supportive Management of
TreatmentTreatment-related Effects
Causes of Taste Alterations
• Damages in taste buds
• Dry mouth
• Oral mucosal infection
• Dental problems
• Chemotherapy side-effects – metallic taste
16
Supportive Management of
TreatmentTreatment-related Effects
Strategies for Taste Alterations
• Recommend tart or sour foods
• Serve cold foods
• Recommend use of plastic utensils if metallic
taste is present
So, what are some of the strategies for improving or
--- improving patient’s outcome for taste alterations?
The recommendations are to serve cold foods,
serve tart or sour foods, also use plastic utensils
instead of metallic to prevent metallic taste, that is.
Recommend rinsing
with salt and soda
mouthwashes before eating and recommending
frozen fruits.
Então, quais são algumas das estratégias para
melhorar ou melhorar o resultado do paciente com
relação
às
alterações
no
paladar?
As
recomendações são a de servir alimentos frios,
azedos ou ácidos e também usar utensílios
plásticos ao invés de metálicos para evitar o gosto
metálico. Recomendar enxaguar a boca com
bochechos de sal e bicarbonato de sódio antes de
comer, e ingerir frutas congeladas.
The other major cancer treatment-related side
effects involve cancer-induced nausea and
vomiting. This affects 70 to 80% of all cancer
patients receiving chemotherapy and 10 to 44%
experience anticipatory nausea and/or vomiting.
Os outros efeitos colaterais relacionados ao
tratamento antineoplásico incluem náusea e vômito
induzidos pelo câncer. Isso afeta 70% a 80% de
todos os pacientes com câncer que recebem
quimioterapia e de 10% a 44% deles experimentam
náusea e/ou vômito antecipatórios.
• Recommend rinsing with salt and soda
mouthwashes before eating
• Recommend frozen fruits
Supportive Management of
TreatmentTreatment-related Effects
Cancer-induced Nausea and Vomiting (CINV)
• 70% to 80% of all cancer patients receiving
chemotherapy experience nausea and/or vomiting
• 10% to 44% experience anticipatory nausea
and/or vomiting
17
Supportive Management of
TreatmentTreatment-related Effects
Incidence of CINV
This is one of the --- illustration or a graph that
shows a study result where the practitioner
prediction of cancer-induced nausea and vomiting is
measured against actual experiences of the patient.
As you can see, the dark orange here has really
significant --- significant incidence of patients having
actual
experiences
after
a
chemotherapy
administration.
Esta é uma das... ilustrações ou um gráfico que
mostra o resultado de um estudo em que a previsão
do médico sobre náusea e vômito induzidos por
câncer é comparada com experiências reais do
paciente. Como podem ver, o alaranjado escuro,
aqui, a incidência de pacientes com experiências
reais após a administração de quimioterapia é
verdadeiramente significativa.
So, what is the cause of cancer-induced nausea
and vomiting? The pathophysiology of emesis is
interesting. And it is theorized as triggered by the
afferent impulses to the vomiting center located in
the medulla from the chemoreceptor trigger zone,
pharynx, and gastrointestinal tract via the vagal
afferent fibers of cerebral cortex. The efferent
impulses are sent from the vomiting center to the
salivation center, abdominal muscles, inspiratory
center, and cranial nerves.
Então, qual é a causa de náusea e vômito induzidos
pelo câncer? A fisiopatologia da êmese é
interessante. E acredita-se ser ativada por impulsos
aferentes enviados ao centro do vômito, localizado
na zona desencadeante quimiorreceptora do bulbo,
à faringe e ao trato gastrintestinal via fibras
aferentes vagais do córtex cerebral. Os impulsos
eferentes são enviados do centro do vômito ao
centro de salivação, aos músculos abdominais, ao
centro inspiratório e aos nervos craniais.
Grunberg SM et al. Cancer. 2004 100(10):2261
Supportive Management of
TreatmentTreatment-related Effects
Pathophysiology of Emesis
• Triggered by afferent impulses to the vomiting
center (located in the medulla) from the chemoreceptor
trigger zone (CTZ), pharynx and gastrointestinal (GI)
tract (via vagal afferent fibers), and cerebral cortex
• Efferent impulses are sent from the vomiting
center to the salivation center, abdominal muscles,
respiratory center, and cranial nerves
18
Supportive Management of
TreatmentTreatment-related Effects
Pathophysiology of CINV
• The CTZ, vomiting center, and GI tract have
many neurotransmitter receptors. Activation of
these receptors by chemotherapeutic agents or their
metabolites may be responsible for chemotherapyinduced emesis.
The CTZ/vomiting center and GI tract have many
neurotransmitter receptors and these are activated
by chemotherapeutic agents or their metabolites.
And they are responsible for the chemotherapyinduced emesis.
Some of the principle
neuroreceptors include serotonin, the dopamine
receptors, and also acetylcholine, corticosteroid,
histamine, cannabinoid, opiate, and neurokinin
receptors.
O centro do vômito ou zona desencadeante
quimiorreceptora (ZDQ) e o trato GI apresentam
muitos receptores de neurotransmissores e estes
são ativados por agentes quimioterapêuticos ou
seus metabólitos. E eles são responsáveis pela
êmese induzida por quimioterapia. Alguns dos
principais
neurorreceptores
são:
serotonina,
receptores da dopamina, além de receptores de
acetilcolina, corticosteroide, histamina, canabinoide,
opiáceos e neuroquinina.
There are different types of emesis. These are
classified into acute onset, which occurs [a] few
moments to several hours after drug administration
and commonly resolves within 24 hours. There is
emesis related --- or described having delayed
onset, which develops 24 hours after chemotherapy
administration, and then anticipatory nausea and
vomiting, which occurs before patients even receive
their next chemotherapy.
Há diferentes tipos de êmese. Classificam-se em:
de início agudo, que ocorre pouco depois ou até
várias horas pós a administração do fármaco e,
geralmente, é resolvido em 24 horas. Existe a
êmese relacionada... ou descrita como tendo início
tardio, que se manifesta 24 horas após a
administração da quimioterapia. Depois, [existem]
as náuseas e os vômitos antecipatórios, que
ocorrem antes mesmo de os pacientes receberem o
próximo ciclo de quimioterapia.
• Principal neuroreceptors involved
– Serotonin (5-hydroxytryptamine [5-HT3])
– Dopamine receptors
– Others include acetylcholine, corticosteroid, histamine,
cannabinoid, opiate, and neurokinin-1 (NK-1) receptors
Supportive Management of
TreatmentTreatment-related Effects
Types of Emesis
• Acute onset – occurs few minutes to several hours
after drug administration and commonly resolves
within 24 hours
• Delayed onset – develops 24 hours after
chemotherapy administration
• Anticipatory nausea or vomiting – occurs before
patients receive their next chemotherapy
19
Supportive Management of
TreatmentTreatment-related Effects
Types of Emesis
• Breakthrough
– Vomiting that occurs despite prophylactic
treatment or “rescue” medication
Another classification is a breakthrough emesis,
which is vomiting that occurs despite prophylactic
treatment or rescue medication. And then a
refractory emesis refers to emesis that occurs
during subsequent treatment cycles when
antiemetic prophylaxis have failed in earlier cycles.
O outro tipo é a êmese intercorrente, que é o vômito
que ocorre apesar de receber [tratamento]
profilático ou medicação de resgate. E, depois, a
êmese refratária refere-se àquela que ocorre
durante ciclos de tratamentos subsequentes
quando da falha da profilaxia antiemética em ciclos
anteriores.
What are some of the important principles on
emesis control? Again, prevention of nausea and
vomiting is the goal. So, the risk of emesis and
nausea for persons receiving chemotherapy of high
and moderate emetic risk lasts for at least four days.
Patients need to be protected throughout the full
period of risk.
Quais são alguns dos princípios importantes no
controle da êmese? Novamente, o objetivo é evitar
a náusea e o vômito. Por isso, o risco da êmese e
da náusea para pessoas submetidas a
quimioterapia de alto e moderado risco emético
dura pelo menos quatro dias. Os pacientes
precisam ser protegidos durante todo o período de
risco.
• Refractory
– Refers to emesis that occurs during subsequent
treatment cycles when antiemetic prophylaxis
have failed in earlier cycles
Supportive Management of
TreatmentTreatment-related Effects
Important Principles on Emesis Control
• Prevention of nausea/vomiting is the goal
• The risk of emesis and nausea for persons receiving
chemotherapy of high and moderate emetic risk lasts
for at least 4 days
• Patients need to be protected throughout the full
period of risk
NCCN™ Guidelines, 2007, www.nccn.org
20
Supportive Management of
TreatmentTreatment-related Effects
Principles of CINV Control
• Oral and IV antiemetic formulations have
equivalent efficacy
• Use the lowest fully efficacious dose of
the antiemetic(s) prior to chemotherapy or
radiation therapy
Some other principles involve oral and IV antiemetic
formulations --- have equivalent efficacy, so we
have to consider that.
Use the lowest fully
efficacious
dose
of
antiemetics
prior
to
chemotherapy or radiation therapy. Consider the
toxicity of specific antiemetics and choice of
antiemetic or antiemetics should be used based on
the emetic risk of the therapy as well as patient
factors.
Outros princípios implicam o uso de formulações
antieméticas IV... apresentam eficácia equivalente,
por isso, temos que levá-las em consideração.
Utilizar a menor dose com eficácia total de
antieméticos
antes
da
administração
da
quimioterapia ou radioterapia. Considerar a
toxicidade de antieméticos específicos e a seleção
de antiemético ou antieméticos que deveriam ser
utilizados com base no risco emético da terapia,
bem como fatores relacionados ao paciente.
Some major classifications of antiemetic therapies
include serotonin, some examples are Zofran and
Kytril; NK-1receptor antagonist or aprepitant; other
non-5-HT3-receptor
antagonists,
such
as
phenothiazines and benzodiazepines.
Algumas das principais classificações das terapias
antieméticas incluem a serotonina. Alguns
exemplos são: Zofran e Kytril; antagonista do
receptor NK-1 ou aprepitanto; outros seriam os
antagonistas de receptores não-5-HT3, como
fenotiazinas e benzodiazepinas.
• Consider the toxicity of the specific antiemetic(s)
• Choice of antiemetic(s) used should be based
on the emetic risk of the therapy as well as
patient factors
NCCN™ Guidelines, 2007, www.nccn.org
Supportive Management of
TreatmentTreatment-related Effects
Types of Antiemetic Therapies
• Serotonin (5-HT3)-receptor antagonists
– Ondansetron
– Granisetron
• NK-1-receptor antagonist
– Aprepitant
• Other non-5-HT3-receptor antagonists
– Phenothiazines
– Benzodiazepenes
21
Supportive Management of
TreatmentTreatment-related Effects
Other Causes of Emesis
• Partial or complete bowel obstruction
• Vestibular dysfunction
• Brain metastases
• Electrolyte imbalance
– Hypercalcemia
– Hyperglycemia
– Hyponatremia
There are some other causes of emesis that could
aggravate or increase nausea and vomiting related
to cancer treatment-related effects. Some of these
factors are partial or complete bowel obstruction;
vestibular dysfunction; brain metastases; some
electrolyte imbalances, such as hypercalcemia,
hyperglycemia,
and
hyponatremia;
uremia;
concomitant drug treatments including opiates;
gastroparesis; and anxiety
Existem outras causas de êmese que poderiam
agravar ou aumentar a náusea e o vômito
associados aos efeitos relacionados ao tratamento
antineoplásico. Alguns desses fatores são:
obstrução total ou parcial dos intestinos; disfunção
vestibular;
metástases
cerebrais;
alguns
desequilíbrios eletrolíticos, como hipercalcemia,
hiperglicemia, e hiponatremia; uremia; tratamentos
medicamentosos
concomitantes,
incluindo
opiáceos; gastroparesia e ansiedade.
So, to summarize, we just discussed some of the
common side effects of anti-cancer treatments
including anemia, neutropenia, mucositis, and
nausea and vomiting. Patients with symptoms of
these conditions need prompt evaluation and
treatment to prevent complications. There are
various supportive care measures available and it is
important to review symptoms and reduce
complications of these problems. So, this is the end
of my presentation and I would like to thank you
very much for your attention. We would appreciate
any feedback as to how this program has helped
you in any way. So, again thank you very much and
send us your e-mail regarding your feedbacks.
Resumindo, acabamos de discutir sobre alguns dos
efeitos colaterais comuns dos tratamentos
antineoplásicos, dentre
os quais, anemia,
neutropenia, mucosite e a náusea e o vômito. Os
pacientes com sintomas dessas afecções precisam
avaliação e tratamento imediatos para evitar
complicações. Existem várias medidas disponíveis
para os cuidados de suporte e é importante
examinar os sintomas e reduzir as complicações
desses problemas. Com isto finalizo minha
apresentação e gostaria de estender meu muito
obrigada pela atenção. Agradeceríamos qualquer
comentário sobre a utilidade deste programa para
vocês. Novamente, muito obrigada e enviem-nos
um e-mail com os seus comentários.
• Uremia
• Concomitant drug treatments including opiates
• Gastroparesis
• Anxiety
Supportive Management of
TreatmentTreatment-related Effects
Conclusions
• Anemia, neutropenia, mucositis and nausea/vomiting
are common side-effects of anti-cancer treatments
• Patients with symptoms of these conditions need
prompt evaluation and treatment
• Various supportive care measures are available to
review symptoms and reduce complications of
treatment-related effects
22