Enviado por
menaribeiro
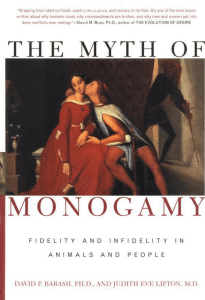
Psychology of sexual response

Psychology of Sexual Response F. Tripodi*, C. Silvaggi*, C. Simonelli** *Institute of Clinical Sexology, Rome **University “Sapienza” of Rome Objectives of the section: To have a basic knowledge of the different theoretical models of sexual response. To understand males and females motivations’ for sexual activity. To learn development stages and changes of sexual response during the life span. To be aware of the relationship between psychological factors (intrapsychic, interpersonal and cultural aspects) and male and female sexual behaviour and response. To consider the comprehensive understanding of sexuality from a biopsychosocial point of view. Introduction “Psychology of sexual response” may be the title for a book and not a chapter. There are so many contributions in the scientific literature about psychology and sexual functioning that any attempt to summarize all the problems in one work and to claim that this be exhaustive, is doomed to fail. Furthermore, this work is limited to the scientific literature regarding the heterosexual population of Western societies. Therefore, the goal in this paper is to give an overall picture of the main issues related to the sexual response which are covered by the big umbrella of psychology (cultural, developmental, intra-psychic, relational, contextual influences). We believe that having a broader view of the factors involved in normal sexual functioning is especially important in the context of a reference volume on sexual medicine, in which the reader's attention may be mainly caught by the dysfunctional aspects of sexuality and their treatment. It seems obvious that psychological and interpersonal factors play a major role in why and how we have sex and, of course, in both the aetiology and maintenance of sexual problems. The ways in which love and affection are expressed in one’s family of origin, the traumatic sexual experiences one has while growing up, the religious, cultural, and societal messages about sex and the ever-increasing impact of the media on one’s beliefs and behaviour, clearly play a role in promoting sexual health or dysfunction. More significantly, individual vulnerability to sexual disruption stems from personality, constitutional/biological dispositions to psychiatric and medical illness as well as from the inability to develop and sustain intimate relationships [1,2]. With the introduction of Viagra [3], professional and public approaches to sexual dysfunctions, and particularly to erectile dysfunction (ED), dramatically changed. Although 1 the bio-psychosocial approach to physical and mental health problems was becoming more accepted, sexual problems had been treated as primarily caused by psychological and relationship factors, with individual, couple or sex therapy the primary interventions. As a culture, we go from one extreme to another [4]. The new, mistaken belief is that sexual problems, especially erectile dysfunction and premature ejaculation (PE), are caused primarily by biological/medical factors and the treatment of choice is a stand-alone medication (frequently prescribed by the patient’s general physician rather than a specialist). This framework was driven by clever marketing strategies by the pharmaceutical industry, physicians lacking sufficient time or interest to grasp the larger picture, and patients who longed for effortless and immediate solutions to complicated life problems [5]. Although experienced clinicians urge physicians to engage in sexual coaching [6] and, in complex cases where medication alone has not been successful, to consult a sex therapist [7], the reality is that most men follow the advice of the marketing ads and feel that all they need to do is ask their physician for Viagra, Levitra or Cialis. Currently, over 90% of men with ED are treated with phosphodiesterase-5 inhibitors (PDE5is) [5]. This has reinforced the “perfect intercourse performance” model of male sexuality [4], which, although it might be functional for single, young adults, probably does not fit mid-life and older adults, especially those who are married or in long-term committed relationships. Likewise, the partner is not immune to the pressures and distress from this emphasis on performance, because she typically experiences any failure on his part as her failure to excite and arouse him. Unfortunately, in only the most difficult, complex cases will the physician suggest a psychosocial assessment and treatment. In this climate, the only role for the woman is to encourage her male partner to admit to a medical problem and seek a medical solution, that paradoxically can reinforce the autonomous and perfect-performance model and alienate her. What surprised many, however, was the large percentage of patients who discontinued pharmacotherapy (dropout rate over 50% [7], a phenomenon not easily explained by the robust efficacy and safety of these drugs. Which factors could influence the dropout rate? The answer lies in the complex inter-relationship between efficacy, treatment satisfaction, adverse events, insurance concerns, cost, and the powerful but often silent multiple psychosocial factors. Medical therapy alone often fails to address these important issues and relapse prevention is usually ignored [1,2,8,9]. We also have to take into account that during the course of the 20th century there was increasing evidence of change in women's expressions of their sexuality, both in terms of their age at first sexual experience, which became progressively younger, associated with a substantial increase in premarital sexual intercourse, and in their increasing engagement in sex as a source of pleasure. We are now confronted with a considerable variability in women's experience of sexual activity and desire for sexual pleasure [10]. Nevertheless, the concept of a variable, flexible sexual response is much easier for the woman to accept because this is more the reality of female sexual socialization and experiences [11]. Most women do not experience high desire at each sexual encounter nor are they expecting to be orgasmic at each encounter. They accept sex being variable both in terms of physical sensations and emotional meanings. However, since the turn of the century, following the impact of Viagra and other PDE5is on male erectile response, attempts have been made to find a “Viagra for women”, with limited success. Moreover, most of the large-scale funded research seeking to enhance female 2 sexual desire has focused on pharmacological interventions, eg. buproprion or flibanserin [12,13] or hormonal treatments such as androgen supplementation delivered via gels, creams, patches, pills or injections [14,15]. Despite the fact that a biological/medical approach to sexual dysfunctions is currently dominant [16], the bio-psychosocial model continues to gain more prominence among researchers and clinicians, conceptualizing the psychological and biological factors as additive and interactive on male and female sexual function and dysfunction. It is hard to establish an effective treatment of sexual problems until we have a better understanding of the normal variability of male and female sexuality. For example, it is now clear that we know little about the nature of sexual desire, which is difficult to define and to measure. Should the sexual frequencies of various sexual behaviours be counted or should attempts be made to assess the degree of internal motivation to engage in sexual activity? Also, the role of hormones remains uncertain. We are becoming increasingly aware of a gap between desire and arousal as sexual experiences and how such experiences are manifested in term of brain action and psychological processes, a challenge that has been particularly emphasized by the advent of functional brain imaging [17,18]. There has been much attention given to possible gender differences in sexual desire [19] and in particular to the concept of “responsive” or “triggered” desire, considered more common in women [20]. The hypothesis that sexual desire and sexual arousal are overlapping concepts rather then describing two distinct phases of sexual response is now stimulating a debate on changes in nosologic categories in the forthcoming edition of DSM V. Other unresolved issues regard the determinants of sexual arousability, of which we still know little, and the interactions between genital response and subjective awareness of sexual arousal [21-24, 10]. Updated models of sexual response suggest that the sexual response of the mind as well as the body has complex and variable patterns, with subjective arousal sometimes preceding sexual desire [25]. Going beyond the study of sexual functioning, as clinicians we are faced with the question of satisfaction: are we able to assess it in patients and to target our intervention taking into account what they need and want? How much importance shall we give to this variable in considering sexual health? We are confronted with people who are unable to achieve subjective sexual satisfaction, despite adequate desire, arousal and orgasm, and there are also problems in defining and measuring this very satisfaction. There is no doubt that satisfaction with one’s sexual life can be independent from sexual activity and the quality of sexual performance, but it does play a role in determining the motivation for engaging in sexual intercourse as well as in causing sexual distress [26-28]. So, Althof et al. [2] challenged us by asking “what should we consider indicative of a successful treatment outcome? Greater frequency of sexual behaviour? More pleasurable activity? Partner or self satisfaction with the degree, intensity and frequency of sexual exchange? Less subjective sexual distress? Changes on a validated assessment instrument?” (page 148) Outcomes conceived solely in terms of the frequency with which partners bring their bodies together, the hardness of an erection, blood flow through the clitoris and vagina, women’s facility in achieving coital orgasm, or men’s prowess at delaying ejaculation, are far too restrictive criteria [2]. It seems better if we assess the complex interplay between the biological, psychological and 3 relational components of individual’s and couple’s sexual lives, paying special attention to help patients in developing comfortable, functional psychosexual skills together with self efficacy, conflict resolution skills and capacity for empathy, facilitating also a serene and effective compliance for medical treatment, in order to enjoy the full benefits of being sexual. Ultimately, sex is a variable and flexible interpersonal process that evolves in a cultural context and not an autonomous process clinging to the criterion of perfect intercourse performance. Moreover, there are many intriguing gender differences in most of the aspects we have considered in this chapter (and we are far from being exhaustive!), but there are surprising similarities between men and women too, that go beyond common stereotypes about sexuality; also, a greater variability among women is noteworthy while that among men is generally still taken for granted, and research has yet to explore many territories. Furthermore, this work is limited to the scientific literature regarding the heterosexual population of Western societies. So, we hope to leave the reader with more questions than answers. He/she is free to choose among the newer scientific proposals in understanding “normality”, and we hope to push him/her to deal with complexity rather than with simplistic points of view. Motivation to sexual activity Human sexuality is motivated by a complex and multifaceted psychology and efforts to reduce sexual motivation to a small number of variables are doomed to fail. Nonetheless, the reasons why people have sex have been assumed to be few in number and simple in nature: to reproduce, to experience pleasure, or to relieve sexual tension. Several theoretical perspectives, well listed by Meston and Buss [29], suggest that motives for engaging in sexual intercourse may be larger in number and psychologically complex in nature. Much of the following contents is based on Meston and Buss’s work. Leigh [30] documented seven reasons for sex: pure pleasure, to express emotional closeness, to reproduce, because a partner wants it, to please a partner, to make a conquest, and to relieve sexual tension. Hill and Preston [31], in their well-known taxonomy, documented eight reasons: to feel valued by a partner, expressing value for a partner, obtaining relief from stress, nurturing one’s partner, enhancing feelings of personal power, experiencing a partner’s power, experiencing pleasure, and procreating. With the exception of ‘‘to make a conquest,’’ most of the recognized reasons for having sex implicitly assume the context of an ongoing romantic relationship or long-term mateship. However, it has also been suggested that humans have a menu of mating strategies, including long-term, short-term, and extra-pair mating [32,33]. Thus, there might be reasons for having sex with a casual sex partner or extra-pair partner, such as the desire to experience sexual variety or seeking to improve one’s sexual skills that differ from those that motivate sex in the context of an ongoing romantic relationship, in which sex might be also used to reward a partner or as a favour in exchange for something the partner has done. Or sex might be used to punish a partner, such as when someone engages in a retaliatory affair in order to exact revenge on a partner for having committed some violation within the relationship [34]. Also, within a stable relationship, sex might be used to intensify the relationship, escalate the level of commitment within the relationship, or turn a short-term 4 relationship into a long-term one [35]. People might use sex as a form of ‘‘mate guarding’’ [36]. This could function in one of several possible ways: to deter the partner from seeking sexual gratification elsewhere or to send signals to potential mate poachers, perhaps by rendering the partner less ‘‘open’’ to extrapair liaisons, causing potential mate poachers to choose other potential targets [37,38]. From perspective on sperm competition [39,40] a man whose partner might have been sexually unfaithful might seek sex, which functions to displace the sperm of the rival male. Or a woman might deplete the sperm of her partner, leaving few available for insemination of rival women. None of these hypothesized functions, of course, need operate through conscious psychological mechanisms. More generally, sex can be viewed as a fungible resource: something that one person has the potential to give and something that another person may want. As a sought-after resource, sex can be exchanged for other resources. Exchanging sex for money, as in the case of prostitution, is one obvious example [41]. Sex could also be exchanged for meat, as it occurs among many traditional hunter-gatherer groups. Sex could be exchanged for favours, special privileges, a preferred job, or indeed for any resource. Finally, the psychology of sex does not occur merely between the individual partners directly involved. Sex occurs within a broader social and cultural context, with implications for prestige, status, and reputation [35]. Having sex with a high status individual, for example, might raise a person’s status within the group. Within some groups, having sex with numerous partners might enhance a person’s reputation, providing the motivational impetus for initiating sex. Sex, of course, can sometimes damage a person’s status and reputation, providing reasons for avoiding it or concealing it from others in the group. In sum, because sex has consequences for status and reputation that can act as incentives or deterrents, a person might be motivated to have sex for social reasons that have nothing to do with the personal relationship within which it occurs. Sexual economics theory assumes that heterosexual communities can be analysed as marketplaces in which men offer women resources such as love, respect, money, and commitment in exchange for sex. In response to economic, political, and other disadvantages, women collectively restrict their sexuality to maintain a low supply relative to male demand, thereby ensuring a high price. Hence, Baumeister and Mendoza [42] tested the hypothesis that sexual norms and practices would be more restrictive in countries marked by gender inequality than in countries where the genders were more equal. An international online sex survey (N>317,000) yielded four measures of sexual activity, and 37 nations’ means on all four measures were correlated with independent (World Economic Forum) ratings of gender equality. Consistent with predictions, relatively high gender equality was associated with more casual sex, more sex partners per capita, younger ages for first sex, and greater tolerance/approval of premarital sex. So, the authors conclude that the idea that collective male power over women leads to collective male sexual gratification appears to be quite wrong. Assuming that men prefer more sex and a sexually freer environment, it is perhaps ironic that they obtain these not by maintaining a dominant control over women but rather by promoting gender equality. The study results suggest that under conditions of high male power, women are not merely passive, pathetic victims but rather respond in an economically rational manner to make the best of their situation. 5 When taken together, all of these diverse theoretical perspectives point to a singular conclusion: the reasons why people have sex are likely to be far more numerous and psychologically complex than taxonomists have envisioned. Meston and Buss [29] published perhaps the most comprehensive exploration to date of the reasons people express for having sexual intercourse, identifying 237 distinct motivations, ranging from the mundane (e.g., ‘‘I wanted to experience physical pleasure’’) to the spiritual (e.g., ‘‘I wanted to get closer to God’’), from altruistic (e.g., ‘‘I wanted the person to feel good about himself/herself’’) to vengeful (e.g., ‘‘I wanted to get back at my partner for having cheated on me’’). One hundred forty-two of them loaded onto 4 primary factors and 13 subfactors that were equivalent in men and women: physical (stress reduction, pleasure, physical desirability, and experience seeking) goal attainment (resources, social status, revenge, and utilitarian), emotional (love and commitment and expression), and insecurity (self-esteem boost, duty/pressure, and mate guarding). The most frequently endorsed reasons for having sex, if taken at face value, reflect what motivates most people most of the time: attraction, pleasure, affection, love, romance, emotional closeness, arousal, the desire to please, adventure, excitement, experience, connection, celebration, curiosity, and opportunity. These were common experiences that may reflect a fundamental universal core of human sexual motivation, a notion that requires cross-cultural research to test. The less frequently endorsed reasons for having sex, however, may be no less important than the commonly endorsed reasons. It is important to note that what constitutes a rare reason for the population as a whole might nonetheless constitute a frequent motivation for a subset of individuals within the population. For example, most people are not motivated to have sex in order to ‘‘get closer to God.’’ But for some people, this has become their cardinal motivation [29]. Gender Differences Regarding gender differences, evolution-based theories suggest that men are more motivated by the desire for sexual variety [43], the chance for an opportunistic copulation [35], the physical appearance of a potential partner [32], and that emotional factors, such as expressing love or intensifying psychological commitment, figure more prominently in women’s reasons for having sex [35]. Some have found that men are more motivated by purely physical reasons, such as physical release or simply because they feel “very aroused”, whereas women are more motivated by emotional reasons, such as to become psychologically closer to a partner [44,45,30]. Others have found that men, more than women, have sex in order to find relief from stress and to enhance their feelings of personal power [31]. Basson [20] described how women might engage in sexual intercourse for the ‘‘spin-offs’’ they receive, such as emotional closeness, bonding, commitment, love, affection, acceptance, tolerance, and closeness. In addition to increasing intimacy with their partner, women may be motivated to engage in sex because they want to increase their own wellbeing and sense of feeling sexually desirable [1,46]. Gliles and McCabe [47] found that whereas attitude to sex correlated positively with spontaneous sexual desire and sexual satisfaction/orgasm, performance anxiety correlated negatively with both of these sexual response phases; so, women with a more positive cognitive appraisal of sexual situations experienced higher levels of motivation to engage in sex. Recently, Carvalheira et al. [48]. 6 described that among women who easily became aroused, 15.5% reported only engaging in sex if they felt sexual desire at the outset whereas 30.7% typically or always accessed desire only once they were aroused. Women in longer-term relationships engaged in sex with no sexual desire more often (42%) than women in short-term relationships (22.4%). The percentage of women that reported fantasies only sometimes was 52.5%. Religion, difficulty in getting aroused, responsive desire, and frequency of orgasm were significantly associated with sexual fantasy. After controlling for age, relationship duration was negatively associated with frequency of initiating sex, women's satisfaction with their own sexuality, and sexual satisfaction with the partner. Meston and Buss [29] found that 20 of the top 25 reasons given for having sexual intercourse were identical for men and women, but despite this similarity, when examining endorsement frequency of reasons, substantial gender differences emerged. Men endorsed reasons centring on the physical appearance and physical desirability of a partner (‘‘The person had a desirable body,’’ ‘‘The person’s physical appearance turned me on,’’ ‘‘The person had an attractive face”) significantly more than women. These findings support the evolution-based hypothesis that men tend to be more sexually aroused by visual sexual cues than are women, since physical appearance provides a wealth of cues to a woman’s fertility and reproductive capacity. Using functional magnetic resonance imaging, Hamann et al. [49] provided neurophysiological support for this notion when they reported greater activation of the amygdala and hypothalamus to visual sexual stimuli in men than in women. Men, significantly more than women, also endorsed reasons indicating experience seeking and mere opportunity (‘‘The person was ‘‘available,’’ ‘‘The opportunity presented itself,’’ ‘‘I wanted to increase the number of partners I had experienced’’). Women exceeded men in endorsing certain of the emotional motivations for sex (‘‘I wanted to express my love for the person’’, ‘‘I realized that I was in love’’). These findings support the evolution-based theory that women, more than men, prefer sex within the context of an on-going committed relationship, and feelings or expressions of love provide signals of that commitment [35, 50]. Also supporting this theory were findings which suggest that sex without emotional involvement was a more powerful motivator for men than for women. Men exceeded women, for example, in endorsing items related to pure physical pleasure, such as wanting to achieve an orgasm, because it felt good, or simply because they felt very sexually aroused. It is important to note, however, that most of the emotional motivations for engaging in sex were not endorsed more frequently by women (e.g., ‘‘I wanted to feel connected to the person’’; ‘‘I wanted to intensify my relationship,’’ ‘‘I desired emotional closeness’’). This finding supports a growing body of clinical evidence suggesting that both men and women at times desire intimacy and emotional connectedness from sexual activity. Meston and Buss [29] also found that men more than women endorsed reasons for having sex that involved a variety of utilitarian functions (‘‘to change the topic of conversation,’’ ‘‘to get a favour from someone,’’ ‘‘to improve my sexual skills’’). These findings contradict the stereotype that women, more than men, use sex to obtain special favours or treatment. Enhancement of social status (boosting reputation, establishing bragging rights, and desiring to tell friends that they had sex with someone famous) seems a male motive for sex rather than a female one. There may be reciprocal links between sex and status: higher status gives men greater sexual access to multiple partners, and having multiple partners or highly desirable sex partners is one means of increasing social status [35]. 7 Although the traditional roles of men as initiators of sexual interactions and women as ‘‘gate keepers’’ may be less a factor today then it was several decades ago prior to the influences of feminism and oral contraceptives, research on college populations suggests that these patterns still exist [51]. The theory of parental investment and sexual selection explains why men express dozens of reasons for having sex at a higher frequency than do women and why men might initiate sex more frequently than women [52]. It also helps explain why parents might socialize their daughters to be more sexually restrained and their sons to be sexually active, a tendency that appears to be universal across cultures [53]. Nonetheless, it is important to bear in mind that there are substantial individual differences within each gender, and women who pursue a short-term mating strategy are especially likely to initiate sex [54, 34]. Although Meston and Buss cited study provided an excellent foundation to begin systematically exploring people’s motivations for sex, more data are needed on how these phenomena operate across the lifespan. It is expected that what motivates women to engage in sex changes across the lifespan as women gain more sexual experience, form more committed and long-term relationships, and experience life changes that undoubtedly impact sexuality such as giving birth, raising a family, and focusing on career goals. The results of a subsequent investigation [55] indicate that women aged 31–45 years have more motives for engaging in sexual intercourse compared with women aged 18–30 years, but the primary reasons for engaging in sex do not differ between the two age bands. Although women’s motivations for sex were quite multifaceted, women aged 18–45 years reported having sex primarily for pleasure, and love and commitment. Regarding men, very recent studies by [56, 57] on male sexual desire and its biopsychosocial determinants showed that cognitive factors (sexual beliefs related to cultural values and automatic thoughts during sexual activity) were the best predictors of sexual desire in men. Specifically, beliefs related to restrictive attitudes toward sexuality, erection concerns, and lack of erotic thoughts in sexual context, had a significant direct effect on reduced sexual desire. Relationship length also predicted lower sexual desire. Age did not show a significant direct effect on sexual desire; it acted indirectly via the presence of restricted attitudes toward sexual activity. Moreover, medical factors did not show a significant direct effect on sexual desire as it is traditionally assumed; rather, they seemed to act through the presence of erection concerns (automatic thoughts during sexual activity), which were strongly related to the presence of medical problems. Psychopathology, dyadic adjustment, and emotional variables (shame and sadness): none had significant direct or indirect effects on sexual desire, after the relative contribution of all predictors was controlled. Sexuality in developmental age Psychological development is an ongoing process that begins before birth and continues throughout life. Over time, individuals either develop or fail to develop numerous sexual and interpersonal capacities, including the ability to love. Sexual identity is a "substructure of sexual functioning" which has been defined in several different ways but with significant conceptual overlap [58, 59], and it is related to: 1. biological sex (male or female); 8 2. gender identity (one's psychological sense of being male or female); 3. gender role (degree to which one adheres to social expectations for one's sex); 4. sexual orientation (the direction and persistence of one's experiences of sexual attraction); 5. intention or values framework (what one intends to do with the desires one has in light of one's beliefs and values). The developmental processes that organize healthy sexuality, while not clearly understood, do not appear to be sexual per se. The quality of attachments to parents, and the ability of caretakers to identify and satisfy the child’s needs interact with constitutional and temperamental forces to foster sexual comfort and identity [60]. In fact, our understanding of sexual development is conceptual and descriptive and is largely devoid of sophisticated evidence-based studies. Freud’s theory of infantile sexuality claims that the small child sucking at his/her mother’s breast experiences a kind of sexual pleasure; such a theory also turned the common understanding of human sexuality upside-down by expanding its definition from a limited biological frame of understanding and placing it on the boundary between the somatic and the psychical. However, it was the concept of attachment and the empirical research tradition to create a new focus for infant studies [61]. Initially, the child was thought of as an essentially passive and/or undifferentiated being from its mother, then the child was seen as checking a sort of "competence", innate firstly and learned later on, in interpersonal relationships. In essence, every human being seems to be modelled by an innate program that is in constant interaction with the "program" of his/her parents, environment and culture [62,63]. Fetal period and first months of life The integration between biological and sensory experience begins in the fetal period and forms the core of body eroticization: the foetus already manifests expressions of pleasure at the fifteenth week, both sucking its finger and swallowing sweet substances that can be injected into the amniotic fluid. The male foetus presents erections starting from a few months before birth; similarly, in one day new-born females, vaginal lubrication and clitoral swelling can be noticed. Research conducted on children still in the uterus and then for one year after birth has shown how much correspondence there is between intra-uterine and extra-uterine behaviour [64,65,66]. The sensory and motor experience of the first months of life is then enriched by the experience of interacting with others early in life that may facilitate or inhibit behaviours related to pleasure in later years. Parent-child contact during physical care, bathing, feeding and play will influence both the future of the child sexual identity, and its ability to establish intimate relationships. The reactions of parents to their child's sexual reflexes are aspects of early sex education: a scandalized or worried parent will communicate distress; on the contrary, a parent who exudes tranquillity and serenity can lead the child to an attitude of acceptance of sexuality. The body gives the child feelings of pleasure and is a useful source of self-knowledge: selfstimulation of genital organs and erogenous zones appears in males around 6-7 months and becomes the prominent to 15-16 months, while it appears later in girls up to 10 months and remains rather intermittent and occasional, with preference for indirect methods, such 9 as rocking or shaking their legs. At age 3, children begin to feel the disapproval of parents for genital games and these activities tend to disappear or to be hidden [67]. Childhood During the preschool period, boys and girls play happily together, and yet there are no sexspecific preferences in the choice of play activities, thus showing a lack of sex role differentiation even in the presence of well-defined gender identity. Thanks to the "matriarchal" context, at this age males still perform with pleasure activities such as sewing, cooking and ironing, daily activities carried out by their reference figures, from which they will distance themselves only in later years. However, since childhood verbal and physical aggressive behaviour is present more in boys than in girls, and the same goes for high-risk behaviour and physically active games. As early as the age of two, a difference in behaviour following the implementation of interpersonal aggression is recorded, with girls showing empathy and seeking reparation contact more often than males [68]. The most frequently reported child sexual behaviours in the study of Sandnabba et al. [69] were characterized by bodily contact, toilet behaviour, sexual interest, self-exploration, genital play and interest, sexual behaviour with other children, sexual verbalization, and voyeuristic behaviour. These behaviours are referred to as “natural and healthy sexual play” and varied according to age. Girls had a higher frequency of domestic and gender role exploring behaviours (more socially-oriented in character, like expressions of endearment towards others, as well as flirtations), whereas the boys tended to engage in explorative acting and information-seeking behaviours (exhibitionistic touching of self, sexual verbalization, a general interest in nudity). Each child develops a gender identity that is a sense of self as being either a boy or a girl and an increasing preference for play, dress, and peer companionship that is perceived by adults as typical or atypical for a child of that gender. Gender conformity throughout childhood is an early developmental marker for adolescent heterosexuality [70]. Childhood gender nonconformity predicts adolescent and adult homosexuality with greater accuracy in boys than it does in girls [71]. Erotic fantasies often appear in the 10th year of life in both genders [72]. These fantasies reflect the formation of the child’s gender identity, sexual orientation and their preferred sexual “script” e.g., what the individual wants to do with another and what they want done to them [73]. Sexually atypical adolescents may become gay or lesbian and in extreme instances may be diagnosed as having a gender identity disorder (transsexualism) or a paraphilia (such as voyeurism, exhibitionism, fetishism, sadism, masochism, paedophilia) [74]. Although there is much speculation about the specific developmental factors that organize children’s gender identity, orientation, and sexual scripts, research has been unable to clarify these developmental processes precisely [75]. In the years before puberty (6-12 years) there are frequent sexual explorations and experimentations, rather than “sleeping sexuality” or latency. In a very interesting study, Larsson and Svedin [76] found that more than 80% of the children had had solitary and/or mutual sexual experiences. Sexual behaviours involving exploration of their own body increased prior to puberty, whereas looking at and exploring genitals together with peers decreased after 10 years of age. Boys seemed to be more active than girls in exploring their own body as well as in exploration together with another child. Solitary masturbation was almost twice as common among boys (62%) than among girls (36%) before the age of 13. 10 Boys reported a more positive attitude to their own experiences, whereas girls, although the majority are also positive, to a larger extent had feelings of guilt. The latter could probably be attributed to different gender socialization, where girls’ sexuality and behaviour are still more monitored and controlled than that of boys are. The girls experimented to a great extent with other girls in their sexual exploration games, a result that may show that samesex games between girls are less threatening and more on equal terms than cross-gender play. Although girls experienced a wide range of consensual activities, they were also more often drawn into non-consensual activities. Two types of developmental factors are thought to increase the likelihood of sexual dysfunction: event-based trauma (single episode) and process-based trauma (ongoing interactions or behaviours) with caregivers [77]. It is reasonable to assume that the remote influences that create sexual dysfunction during adult years do so by triggering old trauma/or anxiety-laden memories, which in the present, are experienced as sexual anxiety. Most predisposing factors to sexual dysfunction are not event-based. Rather, they are process-based, typically involving the ongoing relationship with one’s caregivers. For instance, growing up with parents who express no warmth, do not touch their child affectionately and refuse to acknowledge his/her feelings can inhibit healthy intimate relationships as an adult as well as undermine the child’s self-respect. Negative relationships in childhood may delay or inhibit healthy adult sexual development. Clinicians elucidate the developmental factors that predispose a patient to current sexual dysfunction on a case-by-case basis. Our ideas tend to be based on retrospective patient self-reports; nonetheless, they seem helpful in illuminating both the patient’s and the clinician’s understanding of the problem. Event and process based trauma may explain what causes one person who has suffered adverse circumstances such as unemployment, marital conflict, or infidelity, to become dysfunctional while others under similar circumstances do not [2]. 11 Childhood Masturbation Common features [98, 99]: 1. Episodes of stereotyped posturing of the lower extremities and/or mechanical pressure on the perineum or suprapubic area 2. Associated intermittent (quiet) grunting, irregular breathing, facial flushing and diaphoresis 3. Variable duration of the episode (lasting from a few seconds to several hours) and variable frequencies of episodes (ranging from once in a while to almost continuously) 4. No alteration of consciousness 5. Cessation with distraction 6. The episodes cannot be explained by abnormalities on physical examination. Clinical management: A lack of awareness by the clinical practitioner could result in anxiety for the parents and unnecessary investigations for the child. When there is no evidence of other problems (medical diseases or psychological distress), the clinical practitioner can focus on parental education and guidance. This helps the parents change from viewing their child’s behaviour as evidence of disease to considering it as a harmless habit. Attempts to stop the behaviour immediately are likely to be frustrating and prohibition or punishment of the behaviour tends to reinforce it. It is better to ignore this behaviour or to distract the child during his or her masturbatory activity. When possible, the child should also receive sex information, appropriate for their age. In this way, he/she will learn what is socially accepted and what is not. Although (overt) childhood masturbation often spontaneously ceases eventually, further follow-up is advised. Puberty, adolescence and impact of first sexual intercourse Despite the long-held assumption that puberty provides the crucial trigger for the onset of sexual feelings, more recent research suggests that it is the maturation of the adrenal glands and secretion of adrenal hormones around age 10 that appear to be associated with the development of sexual attraction, thoughts and emotions which are then shaped by cultural expectations of sexuality [75]. For both girls and boys, there is a positive correlation between plasma testosterone levels and increased interest in sex, although this association is stronger in boys than in girls [78]. As their bodies are changing during adolescence, boys and girls receive multiple cultural messages about how men and women do (or should) express, experience and manage their sexual feelings. Notions of men as “naturally” sexually aggressive and women as “naturally” sexually passive may be socially reinforced with the consequence that both boys and girls 12 follow prescribed socio-sexual scripts, i.e. men are sexual initiators and women are sexual gate-keepers [79]. Social pressures appear to have a more significant influence in determining the sexual behaviour of young women than young men (see also paragraph on sexual scripts). Egan and Perry [80] examined the relations between components of gender identity and psychosocial adjustment during preadolescence. The aspects of gender identity assessed were (a) feelings of psychological compatibility with one's gender (i.e. feeling one is a typical member of one's sex and feeling content with one's biological sex), (b) feelings of pressure from parents, peers, and self for conformity to gender stereotypes, and (c) the sentiment that one's own sex is superior to the other (intergroup bias). Adjustment was assessed in terms of self-esteem and peer acceptance. Results highlighted that felt gender compatibility (when operationalized as either self-perceived gender typicality or feelings of contentment with one's biological sex) was positively related to adjustment, whereas felt pressure and intergroup bias were negatively associated with adjustment. In a subsequent study, Yunger et al. [81] confirmed that low gender typicality, low gender contentedness, and high felt pressure all foreshadowed deterioration on one or more indexes of adjustment. The combination of low gender typicality with high felt pressure was especially conducive to internalizing problems, underscoring the importance of the cognitive organization of the gender identity variables. The expressions “sexual fluidity” [82] or “erotic plasticity” [83], suggest that sexual orientation is inherently flexible and evolving over the course of life, so some individuals may experience transitions in sexual orientation during their life (such as during adolescence), referring to their sexual and emotional experiences, their own social interactions and influence of cultural context. Women are considered to be more “erotically plastic” than men and hence to be more amenable to gender and sexual cultural prohibitions and expectations [83]. This may help explain why women tend to have a higher incidence of sexual problems as adults than do men [84]. A first consensual sexual intercourse is often a remarkable and memorable experience in a young person’s life and is typically a rite of passage into young adulthood. Although age of first intercourse and the emotional aspects of the experience are thought to contribute to later sexual functioning, research to date on how the sexual debut relates to adult sexual functioning has been limited and contradictory. Sex therapists often ask their clients about the first intercourse experience as part of their assessment, assuming that a positive or negative experience may impact subsequent sexual adjustment. Despite this clinical application, little systematic information exists regarding contextual factors of first intercourse, the affective salience of the experience, possible effects on sexual attitudes and beliefs, and subsequent sexual development and adjustment [85]. In clinical work it is often reported that traumatic or humiliating sexual initiation and coitus may be associated with later sexual anxiety, aversion and difficulties. Yet, surprisingly, reports that link a negative or disappointing first experience to subsequent sexual difficulties only exist by way of indirect evidence from clinical studies with clients reporting negative first intercourse experiences, as well as current sexual problems [86-88]. Higgins and colleagues [89] indicate that being in a closer, loving relationship is associated with fewer feelings of guilt and more physical and psychological satisfaction for men and, in particular for women. The authors pointed out that gender disparity in sexual satisfaction 13 was large and significant, with men experiencing more psychological and physical pleasure. In general, men ascribe more positive social meaning and report more positive than negative affective responses to first intercourse [90, 91, 92]. For men, first intercourse is considered a ‘‘rite of passage,’’ a ‘‘loss of inexperience,’’ and a part of ‘‘becoming a man’’ [93,94,95]. For women, themes of ‘‘loss of virginity,’’ fears of being stigmatized, and feelings of guilt are more prominent [93, 89, 96]. In a qualitative study of adolescent girls’ first intercourse, Thompson [96] found that the majority of girls in her research remembered their first coital experience as painful and unpleasant. In response, many girls decided to postpone further intercourse for one or more years. The girls who remembered and interpreted the experience positively had mothers who had talked to them about their sexuality in positive ways, had encouraged them to pay attention to their own desire (or lack of it) and had socialized them to expect satisfying sexual experiences. Udry and Billy [97] sampled 1,400 Caucasian adolescent virgins and studied which hormonal and social variables predicted the initiation of adolescents’ sexual activity. They found that for males, free testosterone level rather than social variables was correlated to first coitus, while for females, hormones had no direct effect but most of the social variables did. These included their friends’ sexual activity, grades, deviance, religiosity, sexual permissiveness, parents’ educational level and locus of control. Sexual scripts and cultural influence on sexual response In their groundbreaking work, Sexual Conduct, Gagnon and Simon [100] first applied social scripting theory to human sexuality, noting the similarly between scripts that actors use in theatre and patterned behaviour people engage in sexually. Their theoretical model is perhaps the most cited in post-freudian sexual science. Social scripts may be thought of as both social agents, prescribing what is considered normative within a culture, and as intrapsychic maps, providing directions for how to feel, think, and behave in particular situations [101]. According to Gagnon and Simon’s model, scripts precede the behaviour, in the sense that for the authors there is very little that can be viewed as “spontaneous” in full measure. Today, in the early twenty-first century, Gagnon and Simon's theories [also see 102-105] on the social sources of sexuality may seem commonplace, but they were almost described as the revelation in the late 1970s and early 1980s. At that time, Gagnon and Simon's work on sexuality and social interaction was of crucial importance in developing a fundamentally social alternative to existing biological and psychological models of sexual experience [106]. From their perspective, the subjective significance of sexual life is built up in the flow of social life, in the interaction with other social actors. Gagnon and Simon suggested that perhaps nothing in human life should be thought of as intrinsically sexual; instead, virtually anything can be given sexual significance within a determined social context. For example, lacy lingerie or black leather may indeed incite desire or become the object of fantasy in specific cultural systems, but such desires or fantasies are actually learned responses rather than deriving from intrinsic factors grounded in some kind of underlying human nature. Gagnon and Simon also developed the notion that sexual behaviour is thus socially scripted, that meaningful sexual practices are produced according to socially determined scenarios, 14 rules, and sanctions, which make possible certain understandings of the sexual world while excluding others [106]: “Scripts are a metaphor for conceptualizing the production of behavior within social life. Most of social life most of the time must operate under the guidance of an operating syntax, much as language is a precondition for speech. For behavior to occur, something resembling scripting must occur on three distinct levels: cultural scenarios [paradigmatic assemblies of the social norms that impinge sexual behavior], interpersonal scripts [where social convention and personal desire must meet], and intra-psychic scripts [the realm of the selfprocess]” [107 p. 29]. Interpersonal scripting serves as primary text if only because it is the script that is readable by others; it involves translating abstract cultural scenarios into scripts appropriate for specific and particular situations [108]. Intrapsychic scripts represent the content of mental life and can range from the most orderly cognitive narratives to fragments of desire, memories and future plans [102]. At the interface between the interpersonal and the intrapsychic, the individual is actor, critic and playwright, while the intrapsychic script allows a meaningful internal rehearsal [102,103]. The flexibility of scripts in terms of their internal order and their capacity to be assembled or disassembled in creative or adaptive responses to new life circumstances is a critical element in one’s capacity to manage a changing internal and external environment [109]. It should be noticed that in Gagnon and Simon’s view the term “scripted” cannot be considered a mere synonym or codeword for “learned” [103]; in their perspective, what is conventionally described as sexual behaviour is rooted in biological capacities and processes, but no more so than other forms of behaviour. The script model implies rejecting the idea of a permanent mandate for the sexual rooted in the biological substratum [105], and also accepting the idea that no biological factor can find its way into the behaviour of an individual except through socio-cultural mediation [110]. As well described by Wiederman [101], social scripts are communicated through the examples displayed by members of a culture who have already adopted the scripts and also through mass media depictions of how people act and react in particular situations. In addition, the very structure and the institutions of a society contribute to the formation of scripts, such as in the case of marriage laws and vows and as well as in the case of laws against certain sexual behaviours or certain types of partners. Societal scripts thus specify the appropriate objects, aims, and desirable qualities of sexual interaction, besides providing individuals with instruction as to the appropriate times, places, sequences, and so forth with regard to sexual activity. Wiederman [101] stated that at the individual level, social scripts reduce anxiety by decreasing uncertainty. Sexual scripts provide guidance for the individual, thereby lending sense of predictability as to how the individual should feel and behave as well as to what one should expect from his/her partner. Scripts help answer the question of what particular behaviours mean, whether those behaviours are one’s own or one’s partner’s. Provided both individuals in a sexual couple are following complementary scripts, anxiety is expected to be relatively low. Under these conditions, both partners more or less know what to expect of the other, each shares similar perceptions as to the motives and ascribed meanings held by the other, and a minimal amount of explicit communication or negotiation is needed. Conversely, when both members of a couple hold intrapsychic scripts that are not 15 complementary, predictability diminishes, anxiety increases, and conflict is likely to occur. Individuals tend to rely most heavily on the common elements of social scripts early on in a relationship because they have little information about the idiosyncratic aspects of the other person’s scripts on which to make adjustments. As a couple builds a history together, each partner learns how their sexual scripts overlap and how they differ, and gradually each constructs their own mutually held scripts for sexual activity. However, the period between the start of their first sexual interaction and the time in which an established couple enjoys the comfort of a mutually constructed set of scripts for sexual activity, some degree of disharmony is very likely. There has been research where the script concept was given as the theoretical background [111,108], and studies in which it was more explicitly incorporated [112,113]; however, strong evidence of the script model validity has not yet be found; there are also interesting applications of the script theory in couple counselling and in sex therapy [100] [114,115,101] Some authors highlighted that there is still little understanding as to how scripts work and, in order to solve some issues, it could a large number of psychological mechanisms should be integrated into the model [116]; some other authors critically considered the sexual script approach a good example of a simplified model of reality which lacks taking into account important and highly complex psychological processes [10]; finally, other authors judged the script theory as being more descriptive than explanatory [101, 10]. Male and female sexual scripts Whether men and women differ in their sexuality is often less controversial than the proposed causes of such male-female differences. The two general explanatory camps might be described as polar ends of a continuum. One end is anchored to inherent, biological, or evolutionary explanations, and the other to socialization, cultural, and learning explanations. With regard to potentially sexual situations, scripts provide meaning and direction for responding to sexual cues and for behaving sexually. As men and women exhibit certain differences in sexuality, we might say that the two genders are guided by different but overlapping (and often complementary) scripts. A social scripting perspective allows examining the interconnections within and across each gender’s scripts [101]. Anatomically, boys’ genitals are more easily seen and handled, and this has several (positive and negative) implications. The young boy is taught to hold onto his penis to urinate and to handle it for purposes of washing. Conversely, the young girl is not taught to touch her clitoris, while she is taught to wipe carefully after urination so as not to catch an infection by transferring bacteria from her rectum to her vagina. Thus, boys and girls are given two subtly different sets of messages regarding their own genitals. Boys readily discover that handling their genitals feels good and they are not given the message that their genitals are not necessarily any “dirtier” than other body parts. Differently, girls readily learn that their genitals are difficult, if not impossible, for them to see and that there are “dirty” aspects requiring appropriate precautionary measures. Such anatomical differences and their subtle corresponding messages might help explain why boys typically masturbate more frequently and at an earlier age than girls generally do [117]. In addition, gender roles may encourage sexual exploration more among boys than among girls. Masculine gender roles dictate general independence, assertiveness, and exploration, while feminine gender roles are based more on ideals of behavioural restraint and personal control 16 [118]. It must also be remembered that females can get pregnant, whereas males cannot. Thus, it becomes understandable (though not fair) that parents frequently have a different set of sexual concerns and standards regarding daughters compared to sons. Indeed, research has demonstrated that daughters receive more parental communication about sex than do sons, and most of such communication focus on warnings of risk and danger [119]. This results in women playing the role of sexual gatekeeper in most male-female relationships. Less experience with masturbation, together with ideals based on behavioural restraint and self-protection, set the stage for a relationship-centred set of female sexual scripts. Sexual activity is then viewed as potentially dangerous to a female’s body and to her reputation. As a consequence, there has to be more incentive to engage in sexual activity with a partner than simply seeking for physical pleasure. The result is that female sexual behaviour is framed within the context of a meaningful relationship and is permeated by meanings consistent with that context [120-122]. Young adult men who have not realized how different their female peers’ sexual scripts are from their own, might often be perplexed. At a time when young adults have finally gained a marked increase in privacy from family (such as going away to college or getting married), it often seems obvious to males that sexual activity should “naturally” occur now that a major barrier has been overcome [123]. In a sense, female role allows males to adopt and maintain a relatively unrestrained approach to sexuality in relationships, since it is the female who will limit sex, for both participants’ own good; therefore the male partner is free to focus on outwitting her defences to the extent necessary to achieve sexual activity. In too many cases, male-female differences in sexual roles unfortunately set up a dynamic of polar extremes: the more he pushes for sex, the more defensive she has to be, and viceversa. For many couples, it might seem as though he is obsessed with sex and that she is completely indifferent or disinterested. Social psychology has well-documented phenomena referred to as “the scarcity principle” and “reactance”. The scarcity principle implies that when something is at least desirable in the beginning, the more scarce it is, the more desirable it becomes. Reactance refers to the human tendency to promote a sense of autonomy and independence when confronted with apparent infringement on one’s personal freedom. When applied to sexuality, the above phenomena imply that to the extent that women block men from attaining sexual activity, men will be motivated to increase the value they ascribe to such sexual activity, so that they go to greater lengths to achieve their goals rather than “giving in” to women’s decisions [123] Males and females understandably ascribe different meanings to an initial sexual experience with a new partner. The greater sexual reluctance in women’s sexual scripts makes achieving sexual activity with a new partner all the more rewarding for males. Sexual activity with a new female partner is likely to boost the male’s self-esteem [19], because it makes he thinks that he must have been desirable enough to warrant this new female partner taking on the risks of sexual activity with him in particular. For women, achieving sexual activity with a new partner does not automatically strengthen their self-esteem, because men are thought of as being willing to engage in sex indiscriminately and with little emotional investment; the exceptions would be if that male were of substantially higher status than the female’s previous partners or if the male seemed exceptionally willing and 17 able to invest emotionally in a relationship with her, which implies that she must be more desirable than other women [101]. As to sexual initiation strategies, researchers have found that indirect initiation strategies are more common than direct ones [124,125], and that nonverbal initiation strategies are more commonly used, and viewed as more desirable, than verbal ones [124,126,127]. Data revealed that people found it easier to imagine themselves initiating sexual activity nonverbally as compared to initiating verbally. The ambiguity of indirect and nonverbal strategies may allow an individual to save face in case his or her attempt to initiate sexual activity is rebuffed; however, ambiguity becomes less necessary as a relationship progresses. A preference for indirect and nonverbal sexual communication could also reflect the belief that sexual activity should occur ‘‘naturally’’ and spontaneously [128], that is, without the need for verbal or direct strategies to communicate a desire for sexual activity. Patterns of sexual initiation typically follow traditional gender roles in which men are the initiators of sexual activity and women are the restrictors [129]. Messages about men as the pursuers and initiators of sexual activity and women as targets of men’s sexual advances are quite common in the media, such as primetime television shows [130]. Consistent with traditional gender roles, men report finding it easier to imagine themselves in a situation in which they initiate sexual activity and report greater comfort in the role of initiator as compared to women [131,126]. In addition, women who were asked to describe an ideal or romantic sexual initiation scenario tended to describe their hypothetical male partner as the initiator of sexual activity, and tended to describe themselves as those who controlled the pace of the interaction [112] Seal et al. [132] found that first sexual encounters with a new partner were more likely to be initiated by the male partner, and limited or restricted by the female one, as compared to later sexual encounters with the same individual. The authors suggested that this change reflected a shift to a more egalitarian initiation pattern as a relationship progressed and became more established. Interestingly, although men and women may be relying less on traditional sexual scripts to direct their behaviour, these scripts seem to continue to influence their sexual experiences. In fact, sexual interactions which follow the traditional script and are initiated by the male partner, are rated as more intimate or pleasurable than sexual interactions initiated by the female partner. In their study on strategies used by young adults to initiate sex in the context of a committed relationship, Vannier and O’Sullivan [133] found that men initiated sexual activity more often than women, and this was true for both successful occasions (49% vs. 32%), that is, interactions that led to sexual activity, as well as for unsuccessful occasions, that is, interactions that did not lead to sexual activity (58% vs. 28%). However, it is important to note that although female initiation was less frequent than male one, it still was fairly common. Their findings also make clear that the desire to engage in sexual activity, although not silent, is still expressed with fewer words than actions and that men and women relied on different kinds of nonverbal strategy: men were more likely than women to use indirect nonverbal strategies such as hugging, kissing, or tickling their partners; in contrast, women were more likely than men to use direct nonverbal strategies, such as removing clothing, fondling their partners, or touching their partners’ genitals. Possibly men, as the primary initiators in most relationships, chose more indirect strategies to help offset the chances of rejection from coming on ‘‘too strong’’ or to give women enough time to warm up to sex. 18 Women who feel free to adopt a non traditional initiator role (at least on occasion) may use direct strategies because they are in a context in which they are confident of not being rebuffed, because indirect strategies may be more easily overlooked, or else do not see men as needing time to warm up to the idea of sex. There is also the possibility that men perceive their initiations as beginning at the point when they start kissing or touching and women perceive their initiations as beginning at the point at which they start a more intimate form of sexual activity. Over time, individuals in a committed relationship may refine their ability to read their partner’s signals and may learn how to estimate the likelihood that a sexual initiation will be either welcomed or rebuffed and there is less need to conform to traditional sexual scripts to ensure ease in interactions and shared expectations about one’s sexual role. In short, more established relationships may allow greater freedom to both men and women in initiating sex as they wish. Regarding enactment of sexual scripts during sexual activities, men are expected to play the aggressor, orchestrating sexual performance, as in the expression “making love to” a woman [134]. Women’s roles usually unfold more around being an attractive and seductive stimulus; for example, she may focus on “setting the mood” and wearing sexy lingerie. When sexual interaction actually begins, the man is liable to “take it from there.” The man’s perception of himself as a desirable sexual partner is traditionally linked to his skill as a lover. Such skills may include ability to maintain an erection, delay ejaculation (thereby satisfying his female partner by a long lasting session of penile thrusting), and ideally reading her sexual needs and responding behaviourally. Grace et al. [135] and Potts et al. [136] demonstrated the way in which the default male sexual script (predicated on defining masculine sexuality as active, always desirous, penis-, erection- and performance-focused) has been intensified in the wake of increasing biomedicalization of male sexuality, so that the loss of sexual function becomes synonymous with failure of masculinity or identity itself. On the other hand, the woman’s perception of herself as a desirable sexual partner may include her skill at certain sexual behaviour (e.g., performing oral sex), but it is more likely than male self-perception to include notions of being visually attractive and sexually responsive to his behavioural performance. Wiederman [101] states that the longer that a couple is together, the more likely the male may come to view sex simply as having the meaning it has for him: tension release and bodily pleasure. He may gradually take the maintenance of their relationship for granted, thereby overlooking the possibility that she ascribes different meanings to sexual activity. In couples constrained by traditional gender roles, the female partner may not realize and express her continuing dissatisfaction with the perfunctory, genital-centred sexual encounters to which both members of the couple have grown accustomed. Instead, she may come to define sex narrowly as just that activity she and her partner share. She might then conclude that she is not a very sexual person or that when it comes to sex, she could “take it or leave it.” In contrast, she might feel desire for more non-genital touch and affection, concluding that given a choice between sex and cuddling, she would prefer the latter. It should be noted that, in such cases, if both couple members could view sex more broadly and as involving various forms of giving and receiving physical pleasure, both may view themselves and each other as desirous of sex. 19 Models of sexual response Linear models The four-stage model: Masters and Johnson The first model of sexual function was described by Masters and Johnson in 1966 [137], defined EPOR model. The authors were the first researchers to systematically study the physiology of the human sexual response in men and women in the United States, proposing a linear process characterized by four stages: excitation (E), plateau (P), orgasm (O) and resolution (R) (see Fig. 1 and Tab. 1). According to this model, the sexual response involves a gradual build-up of sexual tension in both sexes, followed by the release of orgasm. Some women, it was noted, are capable of multiple orgasms before resolution. The Masters and Johnson model has been widely accepted and has formed the basis for most subsequent conceptualizations of sexual response in men and women. The model was also used as a framework for understanding common problems and sexual dysfunction in men and women [138]. Fig.1 Tab.1: EPOR Model (Adapted from Masters, Johnson, Human sexual response, Boston: Little Brown and Co., 1966) [137] Male Female Excitement In response to sexual stimuli the process of vasocongestion occurs, where more blood flows into the penis than is flowing out, and the result will usually be that a man will get an erection. How long this takes, and what the erection feels like will differ from man to man, and for the same man over time. Physical changes may include the following: – Changes in the scrotum and testes, with the testes increasing in size and the scrotum elevating, coming closer to the body. Excitement In response to sexual stimuli, vaginal lubrication will usually begin. There are many reasons why women may have less (or no) vaginal lubrication, even when there is excitement and arousal. Other physical changes may include the following: – Vasocongestion will result in the clitoris becoming engorged. – The size and shape of the labia may change. – The inner two thirds of the vagina may expand. – There may be an enlargement of the breasts. 20 – The skin may become flushed, men may experience heightened sensitivity in parts of their body, like the nipples. – Some increase in heart rate, blood pressure, and muscle tension. Plateau Physical changes during this phase may include: – An increase in the size of the head of the penis, and the head may also change color, becoming purplish. – The Cowper’s gland secretes fluid, often referred to as pre-cum, which comes out of the tip of the penis. – The testes move further in towards the body, and increase in size. – There may be a sex flush, muscle tension, increase in heart rate and rising blood pressure. Orgasm During the first stage: – Contractions in the vas deferens, seminal vesicles, and the prostate causes seminal fluid to collect in a pool at the base of the penis, in the urethra (“come” or ejaculate). – This collection is usually felt as a “tickling” type sensation. – In the second stage of the orgasmic phase: – Contractions of muscles occur in a “throbbing” manner around the urethra, and propel ejaculate through the urethra and out of the body. – These contractions (which occur at different speeds, and in different quantities) are usually what are experienced as highly pleasurable feelings of release. Resolution This phase includes: – The loss of the erection as the blood flows out of the penis, which occurs in two stages over the period of a few minutes. – The scrotum and testes return to normal size. – A general feeling of relaxation. There is also a refractory period following ejaculation when a man is physically incapable of getting another erection. This period may last from a few minutes to much longer. It seems to be longer in older men, although there are many possible individual differences. – The skin may become flushed, women may experience heightened sensitivity in parts of their body, like the nipples. – Some increase in heart rate, blood pressure, and muscle tension. Plateau Physical changes during this phase may include: – A continued swelling of the tissues in the vagina, which may be accompanied by contractions of the vaginal opening. – The clitoris can withdraw into the clitoral hood and the external clitoris can shorten in size. – The labia minora increase in size and turn a reddishpurple. – There may be a sex flush, muscle tension, increase in heart rate and rising blood pressure. Orgasm Physical changes involved in female orgasm may include: – Contractions of the pelvic muscles around the vagina. – The uterus and anal sphincter also contract in a throbbing or rhythmic way. – Muscles may spasm, blood pressure and heart rate reach a peak. – The contractions (which occur at different speeds, and in different numbers) are usually what are experienced as highly pleasurable feelings of release. No distinction is made between vaginal and clitoral orgasms in women or orgasm induced through any other form of stimulation. Following one or more orgasms, a gradual return to the pre-stimulated state (resolution) occurs. Resolution This phase includes: – Blood that had engorged areas of the body now flows out, swelling decreases and eventually muscle tension and skin flush go away. – A general feeling of relaxation Despite the enormous influence of the Masters and Johnson model, several limitations and criticisms have been noted [139], especially as far as female sexual response is concerned. First, the model assumes a linear progression of increasing sexual excitement from the onset of stimulation to orgasm and resolution. In this respect, the model fails to adequately describe the highly variable patterns of response seen from one woman to another or even the variability in response from one episode to another, in the same woman. The model is also focused predominantly on the physiologic aspects of sexual response and does not 21 reflect the importance of subjective, psychological, or interpersonal aspects of sexual response. Finally, the model assumes that a sexually functional woman is always responsive to sexual initiation or stimulation, and no indication is given of the importance of sexual desire or libido in their model. Helen Kaplan: the DEOR model In 1974, Helen Kaplan proposed a slightly different model of human sexual response. Her proposal did not result from physiological research in a laboratory, as Master and Johnson’s did, but from her clinical experience as a sex therapist [140]. For Kaplan, sexual response could be understood as involving three key components: Desire Excitation Orgasm Arguably, the crucial piece that Kaplan added to the conception of sexual response was the desire phase (so her model was named DEOR model, i.e. Desire Excitation Orgasm Resolution model). In the earlier model, wanting sex or wanting to be sexual was not a consideration, everything started once someone was already feeling turned on. By focusing attention on desire, Kaplan opened up important discussions about the difference between desiring sex and feeling aroused. Discussion and debate about what defines desire continue to this day [141,142]. More specifically, Kaplan’s first stage of sexual desire consists of physiologic and psychologic components of sexual desire or libido, which are mediated by brain centers in the limbic system but are also influenced, to a degree, by hormonal (i.e., androgenic) and psychosocial influences. The desire phase is viewed as a necessary precursor to the development of adequate excitement and subsequent orgasm in men and women. In Kaplan’s model, although desire is described as centrally mediated, excitement and orgasm are considered as peripherally based processes primarily mediated by centers in the spinal cord. Kaplan’s model was used as the basis for classification of male and female sexual dysfunctions in the third and fourth editions of the Diagnostic and Statistical Manual of Mental Disorders [143,144]. In this model, the sexual response starts with spontaneous sexual desire that is followed by arousal, which may then lead to orgasm and resolution. This model suggests that under normal circumstances, the stages of the female sexual response proceed in direct linear fashion, one stage preceding the next, mirroring the male sexual response. Some authors, [20, 47, 145-147], argued that “linear models” (EPOR, DEOR) have some limitations. In particular, they are based on the assumption of a linear and largely invariable progression of sexual response with parallel processes in men and women. Furthermore, linear models may be more appropriate for men than for women. Finally, phases of sexual response are not discreet, but can be conceptualized as partly overlapping and not always strictly sequential. Newer models emphasize the variability in response from one individual or situation to another and non-linearity that may characterize normal sexual response, above all in women. 22 The circular models Whipple and Brash-McGreer’s Model Some years after, several authors proposed models of sexual response that completely revolutionized the assumptions defined in the previous theories of Masters and Johnson and Kaplan. The first authors who described a new model of circular sexual response pattern were Whipple and Brash-McGreer [148]. They described 4 stages: the first, seduction (encompassing desire); followed by sensations (excitement and pleasure); the third, surrender (orgasm); followed by reflection (resolution). Whipple and Brash-McGreer proposed that satisfying sexual experiences are likely to have a reinforcing effect on women, making them more likely to desire sex, or conversely, to lose desire for sexual activity if their sexual experiences are unpleasant or negative. More specifically, reflection on the sexual experience as pleasurable can lead to the seduction phase of the successive sexual encounter. This model, therefore, acknowledged the cyclic nature of women’s sexual response, although the process of change throughout the various phases in this response cycle did not differ substantially from those in the previous linear models. Moreover, the particular phase descriptions of seduction, sensation, surrender, and orgasm have not been widely accepted as independent phases of female sexual response [146]. It has been recognized, therefore, that the linear models proposed by Masters and Johnson and Kaplan may not fit all women as some may move from sexual arousal to orgasm and satisfaction without any experience of desire, or may experience desire, arousal, and satisfaction without orgasm. Basson’s Model Basson [20] presented an alternative model of women’s normative sexual function that included overlapping phases of sexual response in a variable temporal sequence. In contrast to the prior focus on spontaneous sexual desire, Basson’s circular model of women’s sexual response featured a responsive form of desire, which was accessed once sexual arousal was experienced [47]. This model is based on observations that women experience the phases of sexual response in an overlapping, non-sequential manner that incorporates mental and physical components [149,150]. In this perspective, desire is triggered during the sexual engagement, thereby adding to initial desire. Research confirms that women provide a variety of reasons and incentives for engaging in sexual activity (e.g. desire for increased emotional closeness and intimacy, desire to express love, wish to receive and share physical pleasure, openness to a partner, willingness to be receptive of sexual stimuli in an appropriate context, etc.) [149,151]. According to Basson’s model [20] a woman starts from a state that is desire neutral. If she experiences adequate emotional intimacy from her partner, she may seek or be receptive to sexual stimuli. Receptivity to sexual stimuli allows the woman to move from sexual neutrality to arousal. If the mind continues to process the stimuli onto further arousal, sexual desire will encourage the woman to move forward to sexual satisfaction and orgasm. So, sexual desire is a responsive rather than a spontaneous event. The woman may, at other times, experience spontaneous desire in the form of sexual thoughts, sexual dreams, and 23 fantasies, but at the time of the onset of a given partnered experience, she is likely to be at the “baseline.” Many women who are sexually functional and satisfied do not present the conventional markers of spontaneous sexual desire. Thus, for such women, it would appear that sexual arousal and a responsive-type of desire occur simultaneously at some point after they have chosen to experience sexual stimulation; this choice is based initially on needs other than the desire to experience physical sexual arousal and release. Further arousal follows, generating a focus upon which to build to potential orgasm. Physical well-being may follow without orgasmic release. The rewards of emotional closeness—the increased commitment, bonding, and tolerance of imperfections in the relationship—together with an appreciation of the subsequent well-being of the partner all serve as the motivational factors that will activate the cycle the next time. Any of those potential rewards may be effective on their own, or they may sometimes be accompanied by a physical sexual need or hunger (i.e., the traditional model may sometimes be accurate in situations of partner separation, typically after some days or weeks apart). 24 Basson’s circular model of sexual response (Adapted from Basson R., CMAJ, May 10, 2005, 172/10:1327-1333) [149] Sexual stimuli with appropriate context Psychological and biological processing Willingness to become reptive Spontaneous “innate” desire Motivation Multiple reasons and incentives for instigating or agreeing to sex Subjective arousal Sexual satisfaction with or without orgasm(s) Arousal and responsive sexual desire Nonsexual rewards: emotional intimacy, well-being, lack of negative effects from sexual avoidance In Basson’s model, arousal is conceptualized as a process that is influenced by biologic and psychologic factors. This model assumes that simply because a woman is involved in sexual activity and stimulation this does not mean she is necessarily aroused; her ability to be aroused (her ‘‘arousability’’) may be influenced by factors such as fears of sexually transmitted diseases, past negative sexual experiences and abuse, inadequate birth control, and low self-image [152,153]. If the stimulation is as she wishes, sufficient time is available and she can stay focused, her sexual excitement and pleasure intensify. Clearly, the type of stimulation, the time needed to become aroused, and the context in which arousal occurs are all highly individual. Emotionally and physically positive outcomes will increase subsequent motivation [149]. Compared to traditional models, this circular model of female sexual response cycle considers orgasm and resolution as not being essential. Sexual satisfaction, with or without 25 orgasm, results when the stimulation continues sufficiently long and the woman can stay focused, enjoys the sensation of sexual arousal and is free from any negative outcome such as pain [149]. This emphasis on the subjective nature of sexual satisfaction as opposed to an objective endpoint like orgasm may be more consistent with women’s varied sexual experiences. Feelings of subjective arousal or emotional involvement do not always correlate with physiologic measures of genital congestion. Indeed, emotions and thoughts have a stronger influence on the subjective experience of sexual excitement than does feedback from genital vasocongestion. The model also incorporates biologic, psychologic, and contextual factors in a more comprehensive framework. Finally, the model acknowledges the reciprocal relationship between arousal and desire in women while discounting the previously held notions regarding the primacy of spontaneous sexual desire in women and the necessity of orgasm as a clinical endpoint [146]. This model too has some limitations. As Master and Johnson and Kaplan models, this circular model is based on clinic or volunteer samples [154]. In addition, it could be argued that the shift toward viewing sexual desire in women as being often receptive or responsive in nature, may reinforce negative stereotypes of women as sexually passive or unassertive. Moreover, the model is largely intimacy-based and may exclude some women whose sexual desires and arousal are not intimacy-linked. Nevertheless, by shifting the focus to include subjective and interpersonal factors and by recognizing the nonlinear nature of women’s sexual experience, Basson’s model has contributed greatly to the current understanding of a healthy sexual response in women. Desire and Arousal: how distinct are they in female and male sexual response? According to the Kaplan model, spontaneous sexual desire provides the motive for commencing sexual activity. This type of desire is perhaps best characterized as an apparently innate or spontaneous sense of sexual urging, need, or appetite. Sexual fantasies are often considered to be markers of spontaneous desire and their absence one indicator of dysfunction [144] However, sexual fantasies are not proven to reflect women’s sexual desire [155]. In the Basson [149] composite model, sexual activity may commence for a variety of reasons, not merely (but including) spontaneous sexual desire, and sexual activities may lead to increasing levels of physical and subjective arousal, which may trigger responsive sexual desire. The linear model divides the sexual response into discrete phases that follow one another but do not overlap or occur in unison. The circular model is more flexible in this respect, allowing phases of the sexual response to overlap and merge. From Bancroft and Graham’s perspective [17], sexual desire and sexual arousal are overlapping concepts. As evident in a recent review by Graham [156], whereas this distinction might have some validity when applied to men's sexual experiences, in studies of women's sexuality, there is consistent evidence that desire and arousal are highly correlated constructs [157-159]. Focus groups conducted by Graham et al. [160] indicated that a proportion of women were unable to clearly distinguish between desire and arousal and sexual desire was reported as sometimes preceding arousal and, at other times, following it. Carvalheira et al. [48] reported that more than 30% of the women surveyed, typically, or always, accessed desire only once they were aroused, and for the majority of the 26 participants becoming sexually aroused and being motivated to have sex had equivalent meanings. Regarding arousal, in a series of experimental studies investigating the female sexual response, Laan et al. [161] reported that genital arousal and subjective arousal can be separated. The study results of Chivers and Bailey [162] suggest that the stimuli necessary to produce genital arousal are less specific in women than in men and do not necessarily correspond to women’s sexual orientations, preferences, or subjective experiences of arousal. Moreover, they appear to be prompt automatic reflexes. Recently, the review of Chivers et al. [23] highlighted that the average correlation between genital responses and subjective measures of the sexual response was lower in women (r= 0.26) than in men (r= 0.66). This evidence lends weight to the Basson [163] model, which describes arousal as consisting of physiological (genital and non-genital) and subjective aspects. Both et al. [164] proposed the incentive motivation model, which sees sexual desire as resulting from awareness of sexual arousal or excitement that has already occurred in response to a sexual stimulus, even when the woman is unaware of encountering the stimulus. In this model, both sexual arousal and sexual desire are conceived as responses to a sexually relevant stimulus; internal thoughts or fantasies are considered equivalent to external sexual stimuli in this context. Proponents of the incentive motivation theory argue that there is no such thing as “spontaneous sexual desire” [18] because in order for the sexual system to be activated, the brain has to have processed sexual information. These researchers acknowledge that sexual desire may “feel” spontaneous, but that this is because sexual stimuli are often processed outside of our awareness [165]. So, sexual desire is the result of the interplay between a sensitive sexual response system and stimuli that activate the system. From this notion it follows that sexual desire is not a cause but a consequence of sexual arousal. Bancroft and Graham [17] suggest that for most women, such as those in Garde and Lunde's [166] study, spontaneous sexual desire means desire being experienced not as a response to external cues, but as a result of them thinking about sex and finding the thoughts motivating. This can be contrasted with the situation where a woman thinks about her sexual partner, or even about sexual interaction with that partner, without experiencing any desire; the thought just passes through her mind without initiating a state of “desire.” Looked at in this way, we need to consider what determines whether such a thought does or does not produce an activating effect. This may not depend on the stimulus itself, but on the individual's state of responsiveness at that point in time. This is the distinction that Whalen [167] made between “arousal” and “arousability.” Various factors, independent of external stimuli, can influence an individual's arousability, i.e. their disposition to respond to sexual cues [18], hormones, somatic disease and medication, as well as psychological factors such as stimulus meaning, mood and cognition - and relational context [168, 169]. However, the difficulty that many women have in drawing a distinction between desire and arousal may highlight a deficiency in both the circular and modified linear models of sexual response. It is conceivable that what we refer to as desire is fundamentally the subjective component of sexual arousal. Following this reasoning, apparent spontaneous desire would actually be subjective sexual arousal occurring prior to sexual activities, whereas responsive desire would be subjective arousal occurring after sexual activities have commenced [147]. 27 This matter has caused considerable debate since the publication of the proposed revision of Hypoactive Sexual Desire Disorder (HSDD) and Female Sexual Arousal Disorder (FSAD) into a single “Sexual Interest/Arousal Disorder” for the fifth edition of the DSM [170,171]. Among specialists and researchers there are concerns about this proposal, considered by some as based on theoretical speculations and expert opinions. Thus, in this case, changes in nosologic categories would have risky implications for diagnosis and treatment due to scant empirical evidence for the validity of the single category proposal [see 141,142]. Further data on the relationship between desire and arousal and the difference between women with and without sexual dysfunctions derive from studies on the endorsement of sexual response models. Such studies are dealt with in the next paragraph. Regarding men, sexual arousal has been historically described as a central physiological state, with penile erection in a sexual context as its most valid objective measure [172]. Bancroft [173] defines sexual arousal as a state that is motivated toward experiencing sexual pleasure and possibly orgasm, which involves the processing of relevant stimuli, general arousal, incentive motivation, and genital response. A multifaceted process of male sexual arousal is supported by functional magnetic resonance imaging data indicating different patterns of brain stimulation during sexual arousal, penile tumescence, and penile erection in healthy male volunteers [174]. Furthermore, studies in men without sexual dysfunction have demonstrated that penile erection is not always highly associated with subjective mental aspects of sexual arousal [175]. Based on these findings, a lack of subjective sexual arousal, together with other psychological aspects, may explain why some men with ED fail to respond to treatment with PDE5 inhibitors despite having the physiological ability to achieve and maintain an erection [7]. In line with this, increased interest has developed in the psychological and subjective effects of agents that act on the central nervous system, particularly dopamine agonists and a-melanocortin agonists [176,177], which appear to influence subjective and genital aspects of sexual arousal, as well as to develop scale for assessing subjective male sexual arousal [24]. In order to allow for a comparison with the findings on women reported by Graham et al. [160], Janssen et al. [178] used similar procedures (focus groups) to study sexual arousal and its relation with interest/desire in men. A first conclusion is simple and straightforward: men differ in the importance they attribute to penises, partner characteristics, and to the need for intimacy or interpersonal connection during interactions with a partner. Whereas both scientific and popular discussions of sexual arousal in men tend to emphasize erections, the findings from this study suggest that men experience a wide range of physical (genital as well as nongenital), psychological, and behavioural indicators that characterize sexual arousal. Participants reported that erection was only one of the physiological changes that can be experienced, indicating it as being often present but not as being a necessary condition for the experience of sexual arousal. Also compatible with Graham et al.’s [160] findings in women, this study found that men did not consistently, or easily, separate sexual interest from sexual arousal. Moreover, the results from this study challenge the idea that women are more sexually complex than men, suggesting that men’s sexual arousal is also complex and multifaceted. Men reported that contextual variables, such as ones related to setting or timing, and individual factors, such as the effect of mood, played an important role in their sexual arousal; men in the older age groups reported focusing more attention on psychological and emotional indicators (e.g.: the physical characteristics 28 of their female partner became a less important factor in their sexual arousal, as well as concerns about the number of previous sexual partners that she has had, and the emotional connection with a partner became more important, expressing more confidence in their own sexuality and their ability to please their partner). These findings suggest that it might be both appropriate and conducive to progress in this area of research to re-examine some of our notions about sexual response, putting less emphasis on (while not ignoring) differences between men and women and paying more attention to differences among men and women [178,179]. Women and Men’s endorsement of models of sexual response Some studies compare the extent to which a linear model of sexual response (Masters and Johnson; Kaplan) and Basson’s circular model of female sexual response represent the sexual function of women with and without sexual dysfunctions (SDs). Despite the paucity of empirical data, the Basson’s conceptualization of female sexual response has been widely cited in the female sexual dysfunction literature. Sand and Fisher [180] conducted the first study on this question in a sample of American nurses, revealing that the women surveyed were equally likely to endorse any one of the three sexual response models presented to them. However, over one half of the women surveyed indicated that one or other of the linear models best described their own sexual response, with less than one third endorsing the circular pathway of Basson’s model. So, women do not consistently endorse any single model of sexual response. The circular pathway may be a better representation of the sexual response of women with SDs. Sand and Fisher reported that women with indications of SDs were more likely to endorse the circular pathway of the Basson’s model than were other women. However, evidence to support this is limited. Although Sand and Fisher reported that less than one third of women with SDs endorsed linear models of the sexual response, the proportion of women with SDs who endorsed the circular pathway was also modest: less than 40%. However, it has been suggested that the linear models provided an accurate representation of women’s normative sexual response, while Basson’s model appeared to be a better description of women’s dysfunctional sexual response [180,181] Giles and McCabe [47] found that although the linear model of sexual response was a good fit for women with and without sexual dysfunction, the relationship between sexual arousal and orgasm was mediated by sexual desire for women with SDs. This would suggest that for these women, sexual desire accounts for a significant proportion of the variance in the relationship between sexual arousal and orgasm. This finding is somewhat consistent with data suggesting that women’s progression through the stages of sexual desire, arousal, and orgasm is not a strictly sequential process [182]. Nonetheless, these findings for women with and without SDs indicated that sexual desire typically preceded sexual arousal, rather than subjective sexual arousal triggering responsive sexual desire. Consistent with prior literature emphasizing the substantial overlap between the sexual desire and arousal domains, the study results for the linear model indicated that there was a stronger association between these phases for women with SDs than for women with normal sexual function [182,183]. This association between sexual desire and arousal for women with SDs is consistent with Basson’s representation of the pervasive impact of women’s low sexual desire on their 29 functioning in other phases. These data highlighted that the linear model was a more accurate representation of sexual response for women with normal sexual function, while the circular model was a more accurate representation of the sexual response of women with SDs. However, results support opinion that endorsement of any of the current models of woman’s sexual response is premature [180,47,147]. Regarding men, it has been suggested that linear models may be more appropriate in describing male sexual response [145], but there are no published studies that provide evidence of this. In a very recent study, Sand et al. [184] found that a majority of the men endorsed the Masters and Johnson (48%), or the Kaplan model (39%), whilst a minority endorsed the Basson model (5%) or none of the models (7%). Mean IIEF score was significantly higher in men endorsing the Masters and Johnson and Kaplan models than the Basson model or none of the models (p<0.001). Significantly more of the men without ED (91%) than men with severe or moderate ED (IIEF < 17)(65%) endorsed the Masters and Johnson or Kaplan model (p<0.001). Significantly (p<0.001) fewer men with a history of cardiovascular disease or diabetes endorsed the Masters and Johnson model, while more men in this group endorsed none of the three models. Although these are the first data to assess the proportion of men who endorse different models of sexual response, there is evidence that a majority of men endorsed the Masters and Johnson or Kaplan model, while only a small percentage endorsed the Basson model; significantly more men with ED endorsed the Basson or no model compared to men without ED. Multifactor models A range of sexual response models have been proposed that do not fall neatly into either linear or circular categories. The neurological and biochemical factors that underpin sexual motivation have been the object of some research. Overall, these models endeavor to unify those factors that drive the sexual response, as well as contribute to the development of sexual dysfunction, but are less focused on describing stages of the sexual response per se. In his work over the last two decades, Steven Levine has developed further concepts of sexual drive with sexual desire described as the creation of biological (drive), psychological (motivation), and cultural (values) forces [185]. In 1998, Fisher [186] described the emotion/motivation system whereby basic emotions are seen to arise from distinct circuits or systems of neural activity. She proposed that humans have 3 primary motivation circuits or brain systems that direct behavior. The first influences lust and libido involving estrogens and androgens; romantic attraction is influenced by levels of dopamine, norepinephrine, and serotonin; whereas the third system, involving oxytocin and vasopressin, influences attachment. The evolution of these three emotion-motivation systems contribute to contemporary patterns of marriage, adultery, divorce, remarriage, stalking, homicide and other crimes of passion, and clinical depression due to romantic rejection [187]. There has been criticism of the notion of desire and lust as intrinsic drives. Toates [188], combining the principles of incentive motivation theory and the hierarchical control of behavior for understanding sexual motivation, arousal, and behavior, emphasized the importance of external, (as opposed to intrinsic), sources of sexual motivation and 30 cognitive representations of incentives. The author argued that sexual motivation may emerge through the attractiveness of possible rewards in the environment and that the presence of an incentive can strongly increase the level of motivation directed toward that incentive. In addition, there is evidence that attention to stimuli plays a central role in physiological and subjective sexual arousal [189]. Certain psychological factors (including cognitive distraction and concerns about sexual function) may inhibit the sexual response [190]. Models that explore how information processing may affect sexual arousal have also been developed [191]. The dual control model For the past 10 years, much of the research at the Kinsey Institute has been guided and shaped by a new theoretical model, the Dual Control Model [192]. This postulates that whether sexual response and associated arousal occurs in a particular individual, in a particular situation, is ultimately determined by the balance between two systems in that individual’s brain, the sexual activation or excitation system and the sexual inhibition system, each of which has a neurobiological substrate [193]. This model makes three basic assumptions [10]: 1. although sexual arousal typically occurs in interactions between two or more individuals, and the context and cultural scenario associated with the interaction are important sources of stimulation, both excitatory and inhibitory, the effects of such stimulation depend ultimately on neurobiological characteristics of the individuals involved; 2. neurobiological inhibition of sexual response is an adaptive pattern, of relevance across species, which reduces the likelihood of sexual response, and the distracting effects of sexual arousal and appetite, from occurring in situations when sexual activity would be disadvantageous or dangerous, or would distract the individual from dealing appropriately with other demands of the situation; 3. individuals vary in their propensity for both sexual excitation and sexual inhibition. Although for the majority these propensities would be adaptive or non-problematic, individuals with an unusually high propensity for excitation and/or low propensity for inhibition would be more likely to engage in high risk or otherwise problematic sexual behavior, and individuals with a low propensity for sexual excitation and/or high propensity for sexual inhibition would be more likely to experience problems with sexual response (i.e. sexual dysfunctions). The initial research using this model focused on the male. In order to measure the postulated variance in the two components of the dual control model, a questionnaire was developed and psychometrically established, the SIS/SES, or the Sexual Inhibition Scales/Sexual Excitation Scales [194]. Although the concepts of excitation and inhibition are probably just as relevant to women's sexual responses, and although the SIS/SES questionnaire has demonstrated its value in research in women [195], the measure was originally developed for use in men because the available research underlying the dual control model was largely restricted to the neurophysiology and psychophysiology of male sexual response. Research supported the idea that the SIS/SES questionnaire predominantly measures propensities that are specific to sexual responsivity [196]. The instruments for measuring individual 31 variability in excitation and inhibition propensities have been developed for men and women separately but in each case the authors have adapted the wording to make the questionnaire usable by the opposite sex. Comparison of male and female student samples using the SIS/SES shows significantly higher group means for excitation in men and inhibition in women respectively, as predicted [179]. In a similar comparison using the SESII-W (questionnaire developed for women), significant gender differences were found on all the factors scales [197]. Women were significantly more likely to report that their arousal was enhanced by positive partner characteristics and by hormonal changes. Men, on the other hand, were more likely to indicate a variety of sexual stimuli and negative mood states that could increase sexual arousal. Turning to the inhibition factors, women were much more likely than men to report that sexual arousal was reduced in situations not characterized by trust and intimacy (the relationship importance factor). Women also had higher scores than men on the inhibition factors, ‘Concerns about sexual functioning’ and ‘Setting’; higher scores on these scales indicate that worries about sexual functioning or performance, or about being sexually functioning or performing, or about being seen or heard while having sex are likely to dampen sexual arousal [10]. This model is based on what the Authors regard as the fundamental characteristic of sex, reproduction [17]; for them, reproduction is definitely not a “social construct,” and is the starting point for understanding our varied sexualities. They proposed a male and a female basic pattern, each of which is designed to facilitate a reproductive outcome: the man’s experience being dominated by the pursuit of sexual pleasure, the woman’s by a powerful sense of being desired, and a sense of emotional intimacy, both of which are very rewarding, made possible by her sense of being in control. In both men and women there are other aspects of the experience, called the super-added components, which may be rewarding, but which are not necessary for reproduction. Thus the man may enjoy the emotional closeness, feeling wanted by the woman, or in some sense seeing the experience as formative for an ongoing relationship; such aspects are similar to the components of the female “basic pattern.” The woman may enjoy sexual pleasure from being touched, from having her anterior vaginal wall, or her clitoris caressed, or she may enjoy having an orgasm, all of which are similar to fundamental components of the male “basic pattern.” An explanation for why this distinction between basic and super-added components has not been clearly recognized previously may be that the super-added components for women fit our general ideas of sexual pleasure, whereas their basic pattern is not so explicitly sexual. Conversely, the super-added components of men’s experiences are less readily acknowledged because they are less explicitly sexual. However, all this becomes more relevant when the Authors are trying to understand the variability of women’s sexuality, which presents them with more of a challenge than men’s sexual variability [17]. The Sexual Tipping Point model The Sexual Tipping Point is a model created by Perelman [198], suggesting that a sexual response is determined by a balance between excitatory or inhibitory factors that may be psychological, organic, psychosocial, or cultural. The combined effect of these factors results in a unique threshold or sexual tipping point, which determines whether a sexual response is expressed. According to this model, the sexual tipping point can vary between individuals, as well as within or between sexual experiences of the same individual [147]. 32 The specific threshold for the sexual response is determined by multiple factors for any given moment or circumstance, with one factor or another dominating, while others recede in importance. Perelman says that this model is a useful heuristic device to describe the variety of vectors impacting both normal and dysfunctional response in both women and men [199]. The STP is applicable to sex, which is, almost like everything else, represented by normal distribution curves. These normal models assume that many small and independent effects additively contribute to any observation. As such, sexual attitude, response and behaviour are described with the same familiar curves as all other human characteristics. Perelman argues that arousal is normally distributed like height and weight whereas orgasmic latency is best described by skewed distribution curves like hair and eye colour. Contextual issues and psychosocial issues may affect responsitivity. Psychosocial and cultural influences are complex. As such sexual response not only follows a normal distribution but is also affected by mental and physical factors. As such the aetiology of any dysfunction is typically a combination of both psychogenic and organic factors but the author argues that psychosocial and organic causes can both excite and/or inhibit the final sexual response (see also the dual control model). Positive mental and physical factors increase the likelihood of a response, while negative mental and physical factors inhibit the sexual response. All these factors combine to determine a unique threshold or STP [198]. At rest, the range of sexual response is normally balanced around neutral by these same dynamically opposing inhibitory and excitatory forces and therefore, a given individual is usually neither turned on nor turned off. Recent Developments It has long been argued by commentators, such as Tiefer [200] and Leiblum [201], that the focus on genital response and traditional indicators to sexual desire including fantasies and the need to self stimulate ignore major components of women’s sexual satisfaction with trust, intimacy, and the ability to be vulnerable and receive, respect, communication, affection and pleasure from sexual touching as important factors [202]. The postmodern feminist approach conceptualises sexuality as complex and fluid with rejection of unitary models and so accommodating contradictory representations of experiences and desire. Sexuality is constructed in relation to and interaction with historically and culturally variable social practices such as religion, education and medicine. As such, conceptualising and sexuality are believed to reflect social relations regarding gender, ethnicity, and class and to be culturally managed through the ways women talk, think and practice [203]. The Good Enough Sex Model A recent development which promotes ‘different but equal’ frameworks with 12 dimensions has been described. The 12 dimensions (listed below) are associated with ‘good enough sex’. This emerging concept could be another way forward by providing a framework, which is truly multi-factorial and more likely to establish couple intimacy and satisfaction. Metz and McCarthy [204-206] delineated the principles and sources for the ‘‘Good-Enough Sex’’ model and described its relevance for adult men, women and long-term committed couples. This model emphasizes a psycho-bio-social approach to understanding sexual function as well as assessing and treating sexual dysfunction. The authors argue that the 33 idyllic pursuit of “great” sex is the source of extensive personal dissatisfaction (even agony) and relationship distress, because it amplifies fears of inadequacy and predisposes to lifelong disappointment. There is a “poignant irony” when the pursuit of “great sex” becomes the cause of dissatisfying, dysfunctional sex. In contrast to the ‘‘automatic’’, ‘‘autonomous’’ and perfect intercourse performance model, the Good-Enough Sex model highlights couple intimacy as a cooperative, interactive process not an autonomous one; a variable, flexible, emotionally intimate approach to sexual pleasure and function rather than perfect intercourse performance; that realistically 85% of sex encounters will flow to physically adequate intercourse and when they do not, the couple transitions to an erotic, nonintercourse scenario or a sensual scenario (i.e. cuddling) rather than the demand for intercourse each time; when there is a symptom (e.g. ED), the integration of a medical intervention into the couple’s sexual style rather than as a stand-alone intervention; and the crucial importance of a couple relapse prevention program, rather than treating sex with benign neglect and hoping that symptoms will not return as long as one partner takes medication. Good-Enough Sex recognizes that among satisfied couples the quality of sex varies from day to day and from very good to mediocre or even dysfunctional; that’s why the model intends to replace the prevailing accent on sexual performance to the detriment of sexual quality and satisfaction, advocating a focus on sharing pleasure and enjoying sex function as variable and flexible. Intimacy is the ultimate focus, with pleasure as important as function, and mutual emotional acceptance as the environment. Intimate couples can value multiple purposes for sex and use several styles of arousal. The 12 core premises of “Good Enough Sex” for couple satisfaction 1. Sex is a good, positive element in life, an invaluable part of an individual’s and couple’s long-term comfort, intimacy, pleasure, eroticism and confidence. 2. Sex is inherently relational. Relationship and sexual satisfaction are the ultimate developmental focus and are essentially intertwined. The couple grows as an “intimate team”. 3. Realistic, age-appropriate, accurate and reasonable sexual knowledge and expectations are essential for sexual satisfaction. 4. Good physical health and healthy behavioral habits are vital for sexual health. 5. Relaxation is the foundation for pleasure, function, eroticism, and satisfaction. 6. Sensual touch and emotional pleasure are as valuable as performance 7. Variable and flexible sexual experiences are valuable, abandoning the “need” for perfect performance and adapting with alternate sex scenarios. 8. The five general functions or purposes for sex are integrated into the couple’s sexual relationship for flexibility. In the order of prevalence: • • • • • Physical pleasure (bio-psych) Tension / anxiety reduction (bio-psych) Relationship intimacy (interpersonal) Self-esteem, confidence (psych) Reproduction or procreation (bio) 34 9. The three basic sexual arousal styles (Partner Interaction, Sensual Self-entrancement and Role Enactment) are integrated and flexibly used 10. Gender differences are: Respectfully accepted, embraced & valued. Generously accommodated. Similarities mutually enjoyed. Couple works as an “Intimate Team” 11. Sex is integrated into real life and real life is integrated into sex. Sex is not an isolated fragment of one’s life. 12. Sexuality is often personalized: idiosyncratic spiritual, transcendental, “prayerful” playful, “special” Stressing factors What triggers sexual problems? Problems in sexual function are typically influenced by a variety of predisposing, precipitating, maintaining and contextual factors, shown very clearly in the work of Althof et al. [2], whose footsteps we follow in writing this part. Each of these factors contributes either to both the individual’s and the couple’s ability to sustain an active and satisfying sexual life or to their developing and maintaining sexual dysfunctions. An individual’s vulnerability to later sexual dysfunction is determined by the ratio of risk vs. protective factors as well as their personal resiliency (psychological attribute that describes the individual’s ability to cope with significant adversity or stress in ways that are not only effective, but result in their enhanced ability to confront and master future adversity, Rutter [207]. In general, one’s vulnerability to sexual dysfunction is increased by having more risk factors lasting for longer periods accompanied by greater coerciveness than a single negative or traumatic episode [208]. When stress factors are greater than the individual’s protective factors, then even resilient individuals may be overwhelmed and develop sexual problems. Predisposing factors include both constitutional and prior life experiences that contribute to a person’s vulnerability for dysfunction. However, these factors alone are rarely sufficient to create sexual dysfunction [209]. Negative developmental experiences such as problematic attachments, neglectful or critical parents, restrictive upbringing, sexual and physical abuse and violence, traumatic early sexual experiences as well as a variety of constitutional vulnerabilities are associated with a greater prevalence of sexual dysfunctions and difficulties in adult life. Predisposing Factors (Adapted from Althof et al., 2010)[2] A. Constitutional Factors 35 1. Anatomical deformities, e.g., intersex conditions 2. Hormonal irregularities 3. Temperament, e.g., shyness vs. impulsivity; inhibition/excitation 4. Physical resiliency (a lack of / low) 5. Personality traits, e.g., obsessive- compulsive vs. histrionic B. Developmental Factors 1. Problematical attachment/experiences with parents or parental surrogates 2. Exposure to physical, sexual coercion, violence 3. Surgical intervention/medical illness 4. Event based or process-based trauma 5. Early sexual experiences, e.g., first intercourse 6. Sexual abuse 7. Religious/cultural messages, expectations, constraints Precipitating factors include those more immediate factors that can propel a person from adequate response to dysfunctional response. For any single individual, it is impossible to predict which factors under what circumstances may impair sexual response. Moreover, often there is no clear distinction between either predisposing and precipitating factors or precipitating and maintaining factors. However, there are a lot of studies that provide findings about the relationship between psychological state/traits, sexual confidence, partner issues, couple dynamics and sexual function/dysfunction. Precipitating Factors (Adapted from Althof et al., 2010)[2] 1. Life-stage stressors such as divorce, separation, loss of partner, infidelity, menopausal complaints 2. Infertility or post-partum experiences 3. Humiliating sexual encounters/experiences 4. Depression/anxiety 5. Relationship discord 6. Substance abuse Maintaining factors may prolong and exacerbate problems, irrespective of the original predisposing or precipitating conditions and they are responsible for transforming disappointing or episodic sexual failures into chronic dysfunctions. Maintaining factors include those current conditions that enhance or impede sexual comfort and intimacy. In particular, anxiety, depression and a lack of/low confidence, as well as problems in the relationship, are likely to be responsible for maintaining sexual dysfunction in both men and women. Maintaining factors include immediate contextual factors that influence sexual spontaneity, as well as partner-related factors such as sexual techniques and an absence of sexual dysfunctions. It is obvious that there is reciprocity in partner-related sexual activity such that a problem in one partner may trigger problems in the other and vice versa. It is therefore essential to assess how sexual partners mirror each other in terms of desire, arousal and satisfaction [2]. 36 These factors may not be the ones that initially predisposed or precipitated the initial sexual failure; however, the maintaining factors may be more disruptive to therapeutic outcome than those that initially predisposed the person to develop the sexual dysfunction. Maintaining Factors (Adapted from Althof et al., 2010)[2] 1. Ongoing interpersonal conflict 2. Stress- emotional, occupational, personal 3. Acute/chronic illness/health problems 4. Medications, substance abuse 5. Loss of sexual self-confidence, performance anxiety 6. Body image concerns Contextual factors encompass the every day stresses and demands that impinge on the individual or couple. They are usually temporary but can become chronic and impact on sexual function. Contextual Factors (Adapted from Althof et al., 2010) [2] 1. Present day stresses and demands- financial burdens, unemployment, caretaking of parents, children or partner, fatigue from childrearing 2. Environmental constraints- lack of privacy, time, partners working different shifts 3. Repeated unsuccessful attempts to conceive children, artificially assisted attempts to conceive Body Image Body image appears to be an important factor contributing to sexual self-confidence for both men and women; it impacts both early experiences, (e.g., of being teased), and later sexual experiences with partners. Men tend to worry about penis size, while women tend to worry about body shape and weight. The male is often troubled by concerns that his penis’ size is not good enough to satisfy his partner or himself. He is ashamed to have others view his penis, especially in the flaccid state. Such concerns might be unfounded in reality and might be a presentation of social anxiety or some other clinical problems, such as erectile dysfunction. Concern over the size of the penis, when such concern becomes excessive, might present as the 'small penis syndrome', an obsessive rumination with compulsive checking rituals, body dysmorphic disorder, or as part of a psychosis. However, it is often a worry that can be described as within the normal experience of many men [210]. Men complaining of a small penis despite an actually normal size usually have suffered from this false belief for years and would not be cured just by being told that they are normal. Currently, there is no consensus regarding the most effective approach in managing patients presenting with this complaint. With the worldwide increase in penile augmentation procedures and claims of devices designed to elongate the penis, it becomes crucial to study the scientific basis of 37 such procedures or devices, as well as the management of a complaint of a small penis in men with a normal penile size. In a very recent review of the literature, Ghanem et al. [211] concluded that, according to the available data, most of these men are either misinformed or suffer from a psychological disorder that would not be resolved by surgery. Moreover, based on the current status of science, penile lengthening procedure surgery is still considered experimental and should only be limited to special circumstances within research or university institutions with supervising ethics committees, where a well informed, properly evaluated, and counselled patient accepts the potential risks of the procedure. Many women are sexually self-conscious and many avoid sex when they feel overweight or physically undesirable. Often, these feelings are not based on objective facts, but rather on rigid (Western) standards, culturally imposed, regarding the importance of being young, thin and beautiful. There is little empirical research examining the degree to which an excessive focus on body image interferes with, or contributes to sexual dysfunction, per se, but clinical observations suggest that these preoccupations serve as a distraction during sexual exchanges. Self-acceptance of and feeling comfort with one’s body, irrespective of the degree to which it mirrors cultural stereotypes, is believed to be a salient contributory factor to overall sexual health and function [2]. The context of the romantic relationship also plays a key role: results of the study by Goins et al. [212] indicate that men were more likely to be satisfied with their bodies when they perceived their partners to be so too, when their partners actually were satisfied with their bodies, and when they perceived themselves to have gained relatively little weight throughout the duration of their relationships. Analyses also revealed that men expressed greater body satisfaction when there was a relatively high degree of sexual intimacy in the relationship. Woertman and van den Brink [213] compiled data from 57 studies for a review of empirical evidence regarding the association between sexuality and body image among healthy women. The overall conclusion is that body image issues can affect all domains of sexual functioning. Cognitions and self-consciousness seem to be key factors in understanding the complex relationships between women's body image and sexuality. Body evaluations and cognitions not only interfere with sexual responses and experiences during sexual activity, but also with sexual behaviour, sexual avoidance, and risky sexual behaviour. Pujols et al. [214] found significant positive relationships between sexual functioning, sexual satisfaction, and several aspects of body image, including weight concern, physical condition, sexual attractiveness, and thoughts about the body during sexual activity in women between the ages of 18 and 49 years in sexual relationships. Sexual satisfaction was predicted by high body esteem and low frequency of appearance-based distracting thoughts during sexual activity, even after controlling for sexual functioning status. These findings suggest that women who experience low sexual satisfaction may benefit from treatments that target these specific aspects of body image. Changes in the appearance of one’s body have also been linked to changes in sexual response. For example, women who have undergone psychotherapy for eating disorders that include body–altering components (e.g; weight loss) show enhanced sexual responses following treatment [215]. Worse sexual function correlated with lower body image perception was found in woman with pelvic organ prolapse [216]. Female patients who have undergone treatments involving body–altering surgeries (e.g. for cancer) show a decrease in sexual arousal and interest post-surgery, where predominant concerns, identified in the 38 qualitative analysis of Ussher et al. [217] in women after breast cancer, were emotional consequences, physical changes, feeling unattractive or lacking femininity, reconciliation of self to changes, and impact on partner or relationship. Nevertheless, the conclusion of the recent review by Gilbert et al. [218] was that analyses of sexuality in the context of breast cancer cannot conceptualise the physical body separately from a woman's intrapsychic negotiation, her social and relational contexts, and the discursive constructions of sexuality and femininity. Regarding men, in a very recent study exploring sexual function and body image among long-term survivors of testicular cancer, Rossen et al. [219] found 24% reduced sexual interest, 43% reduced sexual activity, 14% reduced sexual enjoyment, 18% erectile dysfunction, 7% ejaculatory problems and 3% increased sexual discomfort. Seventeen per cent of the patients reported changes in body image, and this was significantly associated with all parameters of sexual dysfunction. Anxiety, depression, personality dimensions and psychopathology The majority of sexually dysfunctional individuals exhibit heightened levels of anxiety suggesting a central role of anxiety in the subjective experience and maintenance of sexual disorders. Correlational evidence exists for the relationship between ED and anxiety. However this does not imply causality. It is also not clear if it is generalized anxiety, or anxiety that is more closely related to the sexual content that is more strongly related to sexual dysfunction in men and women. Laboratory data indicate that the sexual arousal process operates differently in sexually functional and dysfunctional subjects [220]. Contrary to the findings from clinical studies that indicate an inhibiting effect of anxiety, the laboratory evidence has indicated that anxiety (as induced in the lab setting) either facilitates or does not affect sexual arousal in functional subjects. The evidence for sexually dysfunctional subjects is mixed. The cognitiveinformation processing models of sexual anxiety assert that sexual arousal is dependent upon ‘task-relevant’ processing of a sexual stimulus. In sexually dysfunctional subjects, sexual stimuli induce a performance demand, which in turn leads to a shift of attentional focus away from the sexual content of a situation, inhibiting arousal [221]. Activation of the sympathetic nervous system (including anxiety provoking stimuli) facilitates genital sexual arousal in sexually functional women and in women with low sexual desire (but not in women with orgasmic disorder) [222,223]. Overall, the evidence for the role of anxiety in sexually dysfunctional women is mixed, with the suggestion that it is more negative than facilitatory [224]. Whereas moderate levels and relatively ‘safe’ settings may catalyze sexual arousal, higher levels, less feelings of personal control or a longer history of anxiety very likely impair sexual functioning [225] (see also next paragraph on performance anxiety). Depression has a powerful impact on all aspects of male and female sexual response: desire, arousal and orgasm. It is generally agreed that the relationship between depressive mood and sexual dysfunction is bi-directional and further complicated by the sexual side effects of antidepressants [226]. While the exact direction of causality is difficult to ascertain, the data not only indicate a close correlational relationship between depression and sexual disorders but also support a functional significance of mood disorders in causing and maintaining sexual dysfunction. 39 Lykins et al. [227] found that depression was more strongly associated with lower sexual desire in men than in women. Assalian [228] found that men with ED may become depressed because of their sexual dysfunction and because of the secondary effects that ED may have on the relationship. In men who present with one of these two problems it is crucial to ask about the other because of their frequent coexistence. The effective management of depressed men with ED often involves treating both conditions concurrently. Frohlich and Meston [229] looked at the relationship between depression and sexual function in women and results showed that the depressed group reported more desire for solitary sexual activity, a higher frequency of problems with arousal, orgasm and pain, less satisfaction, and less pleasure. Also personality dimensions and psychopathology play an important role on sexual functioning. After controlling for psychopathology, Quinta Gomes and Nobre [230] found that men with sexual dysfunctions presented significantly higher levels of neuroticism when compared to sexually healthy men, neuroticism being the best predictor of sexual functioning. Furthermore, men with sexual problems presented significantly higher levels of depressive symptoms than the controls; depressive symptoms were a significant predictor of sexual functioning as well. Assessment of anxiety and depression should be included as part of the initial evaluation in individuals presenting with sexual complaints and dysfunctions, to ascertain whether possible anxiety/depression is a consequence or a cause of the sexual complaint. If a preexisting acute depression exists, it should be treated along with the sexual problem. Some research suggests that relief of the sexual problem is associated with relief of depression [231]. The role of anti-depressants and anti-anxiety medications as contributory factors to the sexual dysfunction should be evaluated and if implicated, a change in medication(s) may be indicated [2]. In assessing individuals and couples with sexual problems, clinicians often identify the presence of anger in the individuals and relationship. Several clinicians speculated that sexual dysfunction may be a means of expressing anger at the partner; for example, the man’s anger (expressed/unexpressed) toward his partner may be an important intermediate causational factor of delayed ejaculation. Anger acts as a powerful anti-aphrodisiac, and while some men avoid sexual contact entirely when angry at a partner, others attempt to perform, only to find themselves only modestly aroused and unable to maintain an erection/and or reach orgasm [232]. Kaplan [140] stated that the partner rejection, power struggles and sexual sabotage create dysfunction rather than pleasure. Sex therapy cannot be conducted separately from an examination of the couple’s hostility. Exploration of anger must be pursued if treatment is to be successful in the longer term [233]. Alexithymia is a deficit in identifying and communicating emotions that is presumed to play an important role in psychosomatic diseases. Although the influences of alexithymic features on sexuality are still understudied, there are studies in which alexithymia levels were found to be correlates with the severity of ED [234] and of PE [235,236] confirming the importance of the emotive dimension in human sexuality. Performance anxiety, sexual confidence, cognitive factors Performance anxiety is the fear of future sexual failure based on previous failures- a common maintaining contribution for almost all male and female sexual dysfunctions. Many 40 theorists considered performance anxiety to be the central causal factor interfering with sexual arousal since it serves as a distraction from sensual feelings, undermines sexual self-confidence and ultimately, contributes to sexual avoidance, although currently many clinicians consider the performance anxiety as one of the many factors that inhibit sexual response, especially in men [2,237]. The term ‘‘spectatoring’’ means mentally stepping outside of oneself during sexual activity with a partner and monitoring one’s own sexual performance. This detracts attention from the pleasurable aspects of the activity, making it difficult to achieve and maintain sexual arousal, and results in anxiety and heightened performance monitoring. Performance concerns, which trigger spectatoring, thus become self-fulfilling prophecies. Barlow [238,239] also implicated spectatoring as a key factor in the development and persistence of sexual dysfunctions. Barlow’s model proposes that people with sexual dysfunctions may have uncompromising negative schemas about sex (e.g., ‘‘A real man can have an erection whenever, wherever’’) that derive from cultural myths and misconceptions about sex and from a general negative orientation to sexual cues. Sexual schemas that equate sexual performance with gender identity can readily generate anxiety evoking thoughts or spectatoring in sexual situations (e.g.,‘‘Real men don’t lose an erection’’). Sexual activity thus becomes an anxiety-evoking test of manhood. The schema has two important consequences. First, the anxiety evoked by the perceived performance demand gives rise to attentional and information processing biases, which make the person hypervigilant for information that performance is wanting, and threatrelevant cues become an immediate focus of attention at the expense of erotic cues. This distracts the person from the pleasurable and arousing aspects of the situation, which, in turn, makes it more difficult to stay aroused, increasing anxiety further [240]. Second, the schema produces high standards for performance which are seldom achieved, thereby evoking negative expectancies of sexual performance, which, in turn, increase anxiety in sexual situations. Janssen, Everaerd, Spiering, and Janssen [191] similarly argued that when sexual stimuli have other meanings besides sexual ones, processing of non-sexual or emotionally negative meanings can result in low levels of subjective sexual arousal and/or the presence of negative affect. They also propose that people with sexual problems may have broader memories for, and access to, threat- or worry-related information. In turn, worry-related non sexual meaning triggers inhibitory processes and attracts attention away from the sexual aspects of a stimulus. Purdon and Watson’s study [241] on associations between non-erotic thoughts and sexual functioning provides support to Barlow and Janssen models: if the thought is appraised as unpleasant or unwanted, but not especially threatening or relevant to immediate goals, it may give rise to little anxiety, be readily dismissed, and thus not be particularly impairing; if the thought is viewed as threatening, it may give rise to further processing and affective disturbances (anxiety, despair, frustration) that make it difficult to refocus on the erotic aspects of the experience, and/or deploy effective ameliorative strategies to overcome functioning difficulties. As highlighted in this study and in previous ones [242,243], men were more likely to report performance-related thoughts, and women were more likely to report thoughts about body image; while they were equally likely to report thoughts about the external consequences of the activity (e.g., pregnancy, being caught) and the emotional 41 consequences of the activity (e.g., morality, implications of the activity for the relationship). Relationship satisfaction appears to be in itself an important factor in sexual functioning difficulties, mediating the extent to which ambiguous sexual cues are interpreted negatively. The extent to which the man or woman lost, or in some cases never achieved confidence in both their capacity to function sexually, as well as the extent to which they perceive themselves to be a sexual being is given the umbrella term of “sexual confidence”. Althof [244,245] and Perelman [246] emphasized one of the goals for psychotherapy for men with both ED and PE to be the enhancement of their sexual confidence. Although there are now medical treatments for PE, it is important to address the psychological factors associated with this condition, one of which is the level of the man’s diminished sexual confidence. Men receiving sildenafil or tadalafil for the treatment of ED reported significantly improved sexual confidence following treatment [246,247]. Additionally, Phelps et al. [247] found that a combination treatment with sildenafil and a psychoeducational intervention was more likely than sildenafil alone to increase the man’s sexual confidence as well as his satisfaction. To our knowledge, there are no available studies on the association between female sexual dysfunction and the levels of sexual confidence. Several studies have indicated that cognitive factors, such as cognitive distraction, efficacy expectancies, causal attributions, cognitive schemas, sexual beliefs, and automatic thoughts, play an important role in determining sexual response [see 57,249,250]. Results of Nobre and Pinto-Gouveia’s investigation [249] indicated several significant correlations among automatic thoughts, emotions, and sexual arousal. Erection concern thoughts in the men and failure/disengagement thoughts and lack of erotic thoughts in the women presented the most significant negative correlations with sexual arousal. Additionally, sadness and disillusion were positively related to these negative cognitions and negatively associated with sexual arousal in both sexes. On the other hand, pleasure and satisfaction were negatively associated with the above-mentioned negative cognitions and positively associated with subjective sexual arousal in both men and women. Overall, findings support the hypothesis that cognitive, emotional, and behavioural dimensions are closely linked and suggest a mode typical of sexual dysfunction composed of negative automatic thoughts, depressive affect, and low subjective sexual arousal. Relationship Dynamics and Partner’s role The partner’s role as a precipitating or maintaining factor has been overshadowed by focusing on individual medical or psychological factors or on the impact of the quality of the relationship upon sexual function. Clinically, it has been observed that sexual problems are sometimes the cause and sometimes the result of dysfunctional or unsatisfactory relationships. It is often difficult to determine which came first, whether a non-intimate and non-loving relationship, or low sexual desire and/or performance problems leading to partner avoidance and antipathy. The research literature is conflicting, and often difficult to interpret since couples begin therapy with varying degrees of relationship satisfaction or dissatisfaction [see 2]. Several studies consistently demonstrate the interdependence of sexual function between partners. Specifically, they suggest that dysfunction in one partner tends to cause problems for the other and that improvement in function in one partner tends to have a positive effect 42 on the other. Interpersonal factors are frequently cited as one of the causal determinants of low sexual desire, describing HSDD as emerging from an interaction between individual and dyadic characteristics. Notable examples are Talmadge and Talmadge’s [251] relational model, and Rosen and Leiblum’s [115] sexual scripting paradigm. Schnarch [252,253] assumes that sexual desire problems are so widespread as to be normal rather than abnormal, and that these marital impasses are a natural path to relationship growth. Accordingly, HSDD serves as a “distance regulator” in a relationship where there is lack of individual differentiation. McCabe and Cobain [254] found that global deficits in the current relationship were more likely to occur among sexually dysfunctional women than sexually functional women, but found no differences between the two groups in communication or number of arguments. These authors believe that women who are in poor relationships may express their lack of relationship satisfaction by avoiding sexual interactions and restricting their range of sexual experience and intimacy. Among men, however, relationship problems did not appear significantly related to sexual dysfunction, but the level of arguments did. Men with HSDD evidenced more difficulties than non-HSDD men in their level of relationship functioning by demonstrating increased arguments and lower sexual satisfaction. Hurlbert et al. [255] found that the relationship between HSDD and relationship functioning was stronger for women than for men. A large scale health and sexuality survey of 2,050 women between the ages of 20-70 found that those women who reported lowered levels of sexual desire also reported more relationship dissatisfaction, lower frequencies of sexual activity, fewer orgasms and more distress [256]. Kelly et al. [257] found that among couples where the female was experiencing orgasmic disorder, the couples experienced poorer communication than control couples who did not experience any sexual dysfunction. Oberg and Fugl-Meyer [258] found that the major predictors of female sexual dysfunction were dissatisfaction with the relationship and partner sexual dysfunction. Atwood et al. [259] also emphasized the importance of the couple relationship in both the development and maintenance of ED. Rosen and Althof [260] found that PE impacted on both the men and their partners. Couples who have been sexually abstinent for several years often adapt to life without sex. The Index of Sexual Life (ISL) developed by Chevret et al. [261] indicated that the partners of men with ED reported a significantly decreased sexual drive and sexual satisfaction, compared with partners of men without ED. Fisher et al. [262] in the FEMALES study reported a decline in sexual desire, arousal, orgasm frequency and satisfaction among female partners of men with ED, compared with their sexual functioning before their partner developed ED. Studies have shown that the participation of the partner supports the adherence to therapy, and her involvement facilitates successful long term ED therapy. These studies suggest that women should be included in ED treatment if possible [263,264]. Moreover, the presence of the couple ensures not only the restoration of erectile function but improves the quality of sexual life of both partners [264]. An interesting finding by Smith et al. [265] was that the partners of men with Chronic Prostatitis/Chronic Pelvic Pain Syndrome also experienced low levels of sexual functioning and sexual satisfaction, as well as poor relationship functioning. In fact, male sexual 43 functioning significantly predicted the sexual functioning of their female partner. Clinicians and researchers have noted that these relationship problems are often not well addressed in the treatment of sexual dysfunction in both men and women [266]. The data strongly support the view that clinicians should take a biopsychosocial approach to the treatment of sexual dysfunctions and include evaluation of the partner if possible. Treatment focused solely on the sexual dysfunction is likely to fail if the underlying relationship dynamics are ignored; without treating the problematic relationship, enhanced sexual function is likely to be temporary or that other psychological symptoms in one or both partners will develop in order to maintain homeostasis. While there are conflicting findings, the preponderance of evidence suggests that therapy, which specifically addresses relationship issues, will be more successful than therapy that only focuses on the resolution of the sexual dysfunction [267]. Stravynski et al. [268] conducted a study to determine if treatment outcome for sexually dysfunctional men differed depending upon whether therapy focused on sexual problems, interpersonal issues, or a combination of both. The results demonstrated that a focus on the interpersonal issues was more effective than the other two treatments. In a subsequent study of sexually dysfunctional women, Stravynski et al. [268] found that treatment focusing on the resolution of sexual problems or relationship problems were equally effective compared to a control condition in resolving sexual problems at both post-treatment and 12 month follow-up. In contrast to the above findings, Hawton, Catalan, and Fagg [269] found that the quality of the couples’ relationship was not related to successful treatment outcome for women presenting with low sexual desire. The most important predictor of success was the male partner’s motivation to obtain a successful outcome at the beginning of therapy. Consistent with the importance of the partner in treatment outcomes, Sand et al. [270] found that men with ED rated their relationship with their partner higher than many other aspects of their lives (e.g., employment, material possessions). These findings highlight the importance of interpersonal relationships in managing ED. In a series of case studies, Leiblum [271] and Althof [7] both found that although oral medication (e.g., sildenafil citrate) may assist a man in obtaining an erection, the use of this intervention was unlikely to lead to a satisfying sexual relationship unless relationship issues were also addressed. These issues include feelings of insecurity that develop as a result of the sexual dysfunction, as well as anger and disappointment. Returning to an active sexual life after an extended period of sexual abstinence requires more than medication alone. The authors highlighted the importance of obtaining a thorough assessment and treatment of both the interpersonal and sexual relationship as well as including the partner, where possible, in the therapy process. While it is impossible to determine cause and effect relationships with any certainty, the literature suggests better long-term outcome when relationship issues are treated and resolved [235,244,272]. Whether the relationship problems preceded the development of the sexual dysfunction, or vice versa, it would appear that the most effective form of intervention is to treat both the relationship and sexual difficulties. If this does not occur, the problem that is not addressed may continue to influence the other area that is the focus of treatment, and thus may eventually undermine the treatment process [2]. 44 Sexuality and ageing The increasing proportion of over-65s in the last decade is a pattern seen in many different countries all over the world (from Japan to Italy, from UK to the United States) and these figures are expected to continue rising [273,274]. Despite the existence of a large body of medical literature on sex and ageing, psychological literature on this topic is very scarce [275]. The available studies suggest that increasing age is associated with a decreased interest in sex; despite this, research also demonstrate that interest in sex among elderly has increased over the last 10 years. A substantial proportion of elderly men and women consider sex to be an important part of their life (Hyde et al., 2010; Woloski-Wruble et al., 2010). Due to the growing rate of healthy people in their third age who recognizes the importance of sexual health, it is necessary considering those factors that could affect sexual life. There is no doubt that in their third age men and women undergo many biologically and psychologically related changes that affect sexual functioning (e.g. hormonal changes, relational pattern modifications), but whether or not these are experienced problematically will depend upon some important variables [276-280]: – whether they are sexually active (often related to marital status like widowhood); – the types of sexual activity they engage in (sexual behaviour patterns: touching, precoital sexual activities); – the socio-cultural background (sexual education: norms and roles, such as genderspecific roles, mid-life crisis); – relational status (presence of a sexual partner as a protective factor, experience of separation); – psychological well-being (depression, anxiety, personality characteristics as dependence and obsession, psychological flexibility as well); – physical health (organic metabolic disease: vascular, hormonal, iatrogenic). Satisfaction level for sexual life is related to some factors: – – – – satisfaction level for sexual life over previous years; ability to reach orgasm; good and open communication with partner; overall satisfaction with life: characterized by elements like working outside of own home, having partner and children, good levels of education, being healthy. [28,277,281-283] As with all age bands, there are multiple variables linked to sexuality in elderly people, due to a complex interaction between psychological and physiological functioning, to the extent that a bio-psycho-social and multidisciplinary approach is required [273]. In considering the 45 elderly patients clinicians have to separate those elements that are attributable to “normal” ageing from those that are linked to an unhealthy condition. Health professionals have to become pro-active in designing and implementing interventions in order to promote sexual health [281]. Sexual counselling should be oriented on: 1. showing availability, with emphatic attitude, to speak and answer to questions about changes in sexuality, if it is patient’s desire and interest ; 2. verifying that the patient wishes treat sexual dysfunctional aspects; 3. providing some information; 4. giving specific suggestions; 5. referring to specific therapy, if needed (e.g. inform the patient about possible treatments for sexual dysfunctions); 6. being ready to accept and manage the patient’s feelings of sadness over the changes that are not reversible (or at least on the possibility that they are not). It is necessary to develop more appropriate strategies that will enable health-care professionals to discuss the subject of sexual function with their patients, offer them conditions that will allow them to exercise their sexuality fully and pleasurably [284]. Doctors are very well placed to affirm the value of fulfilling sexual relations for older patients, but professionals are often uncomfortable about asking patients questions regarding sexual activity; many old people hope that they can raise the subject during a consultation, although it is often presumed that ageing patients do not engage in sexual activity, especially if they do not have a partner [274,285-287]. On the other hand, due to their feeling that no other one is experiencing such interest, worries about doctor’s judgment (as being considered a “sex maniac” or “abnormal”), concerns about wasting the doctor’s time [273, 288] seeking treatment for sexual issues is often inhibited and embarrassing [289]. It seems that older people may also internalise the stereotype of sex in older age as being “wrong” or “inappropriate” (the Geriatric Sexuality Syndrome as coined by Kaas, [290]). At the same time, Health Care Providers (HCPs) find it really difficult to talk about sexual topics, they feel under-trained in this area and often stereotypes based on personal beliefs emerge. Although it is important to keep in mind the delicate issue on sexuality in elderly, at the same time doctors must be careful not to over-sexualise the ageing process, nor to over-medicalize declining sexual functioning and interest. It may be a right choice to start the conversation with the patient by asking him/her permission to talk about more personal issues. Lastly, a cultural change is necessary, as well as promoting campaign to increase awareness in older age and improving communication skills, in both patients and HCPs. As reported by Taylor and Gosnet [273], recommendations for HCPs include: 1. 2. 3. 4. verifying there is enough time to discuss the issue; respecting the need of privacy; not discussing sexual themes if patient’s adult children are present; offering an appointment with a doctor of the same sex if requested by patient, and when possible; 5. investigating “lifestyle factors” (e.g. smoking, drinking, health status) affecting 46 Conclusion Throughout this chapter the reader has encountered a lot of theories and models aimed to structure our thinking on human sexuality and to suggest some indications for reading normal and dysfunctional sexual responses. Perhaps the reader might feel somewhat frustrated to know how many questions among those emerging at least from the last decade research, have remained unresolved. However, we consider this uncertainty as a great opportunity for young scholars and specialists in sexual medicine to rise challenges, to encourage their thinking and curiosity. The challenge facing researchers is not only to design studies that meet the highest level of evidence-based medicine but to also demonstrate concern for the complexity of sexuality, in other words, to examine how human sexuality as experienced and expressed. A narrow mechanistic focus on genital function/dysfunction or successful/unsuccessful performance fails to encompass the broader variables that constitute sexual response. A lot of information derives from various surveys carried out in modern Western societies; such surveys usually reflected prevailing concerns or problems (i.e., premarital sex, teenage pregnancies, STIs and AIDS, etc.) [10]. The first exception was Kinsey [291,293], with his groundbreaking studies of the sexual experience of ordinary men and women, and whose first goal was to demonstrate the extraordinary individual variability in human sexuality: no two people were the same, and when one looked at the distribution of sexual characteristics, there were no obvious cut-offs that would justify the concept of “normal” versus “abnormal”. This was his most important challenge to both scientific and public opinion [293]. One of the lessons from Kinsey’s research is that, typically, there is a discrepancy between what people do sexually and what society assumes and expects them to do. Whereas, before Kinsey’s contribution, the assumptions were more restrictive than the reality, with the commercialization of sex, in particular to increase magazines sell, after Kinsey there has been an increasing tendency to “sell” the idea that people are more sexual (and also have to look younger) than they are in reality [10]. If we consider Kinsey’s publications as one of the most interesting milestones of modern sexology, it is surprising to realize that we are still now trying to find evidence regarding individual variability in sexual response and that the study of “normality” is still an open challenge in today scientific landscape. The 90s of last century saw both the beginning of the “Viagra era” and the evolution of the debate to overcome the biology-culture dichotomy through a paradigm shift to a broader interdisciplinary study of human sexuality [294]. There is general agreement that the complexity of sexuality, whether normal or dysfunctional, is created by the interaction of the forces between culture, individual development, individual 47 psychology, interpersonal relationships and biology. There is no sexual behaviour, solitary or partnered, is not shaped, in some way, by each of these influences. This is especially true since sexual behaviour most often occurs in a dyad with two individuals, each bringing their unique histories, inhibitions and motivations to sexuality [2]. Nonetheless, the pharmacological revolution has exposed clinicians and researchers to the risk of separating body and mind and to the risk of developing a “sexual medicine” following a linear approach to the understanding and treatment of sexual problems, focused only to restore sexual functioning in a predefined pattern of normal response. The failures derived from sequential approaches and the sharp division of languages and skills of different specialists, have increasingly led professionals to suggest treatments of sexual dysfunction involving the integration of models and techniques [9,295,296]. Combination or integrated treatment is the logical extension of the biopsychosocial model. It addresses the relevant biological/medical and psychosocial issues that predispose, precipitate and maintain sexual dysfunction. Too often, medical treatments for sexual dysfunction, both those approved and those off-label, are narrowly or mechanistically directed at sexual function alone and fail to address the salient psychosocial issues that hinder treatment efficacy, satisfaction and compliance. Likewise, psychological intervention alone may be time consuming, costly and may fail to yield rapid symptom improvement [2]. Combined or integrated treatment paradigms challenge traditional sex therapy practices, providing a venue where the psychosocial factors can be identified, acknowledged and addressed to ensure that change is genuine and resilient, while the patient simultaneously makes use of and has success with a variety of efficacious medical treatments for sexual dysfunction. Moreover, therapy should be tailored for each patient, as one treatment does not fit all. Each treatment option should be discussed with the patient including the success rate and possible adverse effects so that the patient participates in the decision-making. This will improve compliance and therapy success [235,297]. Last but not least, the effectiveness of any intervention may depend on the skills of the clinician delivering the intervention; this is in turn influenced by previous training and ongoing supervision of the individual sex therapist [8]. In spite of a growing demand for help in the sexual field, there is paradox regarding the professional figure of the sexologist. In many European countries neither a specific university degree nor a professional register exists, so the position of the sexologist is that of title without legal protection. Even more at risk is the status and professional practice of sexologists who are not physicians [8,298,299]. Sexology sometimes appears as a part of some specialization courses in the Faculty of Medicine, or as an exam in the Faculty of Psychology. Therefore, professional training in this field is traditionally left up to the initiative of private institutes or associations, that “independently” establish the training requirements for the figures of sex educator, sex counsellor, clinical sexologist or specialist in sexual medicine. As a result, nowadays, any physician or psychologist can treat sexual problems, even without specific training or affiliation to an association in the field. Establishing standard criteria of appropriate training is therefore another important challenge that the most prestigious sexological associations are still facing. Physicians and mental health professionals, of course, cannot have the same ability in dealing with biological, cultural, interpersonal, and individual psychological aspects of a given dysfunction, but specialists in sexual medicine are required to be wary of against 48 simplistic thinking regarding the cause and treatment of any sexual problems. There is a vital need for collaboration between clinicians in the evaluation, treatment and education surrounding sexual dysfunctions. Each discipline has something to contribute to patient care [2]. Our experience highlights that clinical sexology still has a long way to go before achieving a productive integration between specialists involved. Integration is easier and already welltested in private practice [8]. Hence, we believe that it is necessary to continue to work in a common effort and disseminate a sexological culture characterized by a holistic view of sexual health. References 1. Althof, SE, Leiblum, SR, Chevret-Measson, M, et al. Psychological and interpersonal dimensions of sexual function and dysfunction. J Sex Med 2005; 2: 793-800. 2. Althof, SE, Abdo, CH, Dean, J, et al. International Society for Sexual Medicine's guidelines for the diagnosis and treatment of premature ejaculation. International Society for Sexual Medicine. J Sex Med 2010; 7: 2947-2969. 3. Goldstein, I, Lue, T, Padma-Nathan, H, Rosen, R, Steers, W, Wicker, P. Oral sildenafil in the treatment of erectile dysfunction. N Engl J Med 1998; 338: 1393– 1404. 4. McCarthy, B, Metz, M. The “Good-Enough Sex” model: a case illustration. Sex Relat Ther 2008; 23: 227–234. 5. Althof, S. Sex therapy in the age of pharmacotherapy. Annu Rev Sex Res 2006; 17: 116-32. 6. Perelman, M. Sex coaching for physicians. Int J Imp Res 2005;15 (Suppl. 5); 67–74. 7. Althof, S. When an erection alone is not enough; biopsychosocial obstacles to lovemaking. Int J Impot Res 2002; 14 (Suppl.1): S99-S104. 8. Simonelli, C, Fabrizi, A, Rossi, R, Silvaggi, C, Tripodi, MF, Michetti, PM, Clinical sexology: An integrated approach between the psychosomatic and the somatopsychic. Sexologies 2010; 19: 3-7. 9. McCabe, M, Althof, SE, Assalian, P, et al. Psychological and interpersonal dimensions of sexual function and dysfunction. J Sex Med 2010; 7: 327-36. 10. Bancroft, J. Human Sexuality and its Problems, 3rd edition. Churchill Livingstone Elsevier: Edinburgh, 2009. 11. Heiman, J. Orgasmic disorders in women. In: Leiblum, S, ed. Principles and practice of sex therapy (4th edition). Guilford: New York, 2006, pp.84–123. 12. Segraves, R, Croft, H, Kavoussi, R, et al. Bupropion sustained release (SR) for the treatment of hypoactive sexual desire disorder (HSDD) in non depressed women. J Sex Marital Ther 2001; 27: 303-316. 49 13. Goldfischer, E, Breaux, J, Katz, M, et al. Efficacy of continued flibanserin treatment in premenopausal women with hypoactive sexual desire disorder: Results from the Rose study. J Sex Med 2009; 6: 45. 14. Shifren, J, Braunstein, J, Simon, J, et al. Multi-center, double-blind, placebocontrolled evaluation of transdermal testosterone replacement in surgically menopausal women with impaired sexual function. N Engl J Med 2000; 343: 682688. 15. Davis, S. Testosterone treatment: Psychological and physical effects postmenopausal women. Menopausal Medicine 2001; 9: 1-6. 16. Rowland, D. Will medical solutions to sexual problems make sexological care and science obsolete? J Sex Marital Ther 2007; 33: 385–397. 17. Bancroft, J, Graham, CA. The varied nature of women's sexuality: unresolved issues and a theoretical approach. Horm Behav 2011; 59: 717-729. 18. Laan, E, Both, S. What makes women experience desire? Fem Psychol 2008; 18: 505–514. 19. Baumeister, RF, Tice DM. The social dimension of sex. Allyn & Bacon: Boston, 2001. 20. Basson, R. The female sexual response: A different model. J Sex Marital Ther 2000; 26: 51–65. 21. Apfelbaum, B. Retarded ejaculation: A much-misunderstood syndrome. In: Lieblum, SR, Rosen, RC, eds. Principles and practice of sex therapy: Update for the 1990’s 2nd edition. Guilford Press: New York, 1989, pp.168-206. 22. Chivers, ML, Rosen, RC. Phosphodiesterase type 5 inhibitors and female sexual response: faulty protocols or paradigms? J Sex Med 2010; 7: 858-872. 23. Chivers, M, Seto, MC, Lalumiere, ML, Laan, E, Grimbos, T. Agreement of selfreported and genital measures of sexual arousal in men and women: a metaanalysis. Arch Sex Behav 2010; 39: 5–56. 24. Althof, SE, Perelman, MA, Rosen, RC. The Subjective Sexual Arousal Scale for Men (SSASM): Preliminary development and psychometric validation of a multidimensional measure of subjective male sexual arousal. J Sex Med 2011; 8: 2255–2268. 25. Basson, R, Leiblum, S, Brotto, L, et al. Revised definitions of women's sexual dysfunction. J Sex Med 2004; 1: 40-8. 26. Bancroft, J, Loftus, J, Long, JS. Distress about sex: a national survey of women in heterosexual relationships. Arch Sex Behav 2003; 32: 193-208. 27. Philippsohn, S, Hartmann, U. Determinants of sexual satisfaction in a sample of German women. J Sex Med 2009; 6: 1001–1010. 28. Dundon, CM, Rellini, AH. More than sexual function: predictors of sexual satisfaction in a sample of women age 40-70. J Sex Med 2010; 7: 896-904. 29. Meston, CM, Buss, DM. Why humans have sex. Arch Sex Behav 2007; 36: 477-507. 30. Leigh, BC. Reasons for having and avoiding sex: Gender, sexual orientation, and relationship to sexual behavior. J Sex Res 1989; 26: 199–209. in 50 31. Hill, CA, Preston, LK. Individual differences in the experience of sexual motivation: Theory and measurement of dispositional sexual motives. J Sex Res 1996; 33: 27– 45. 32. Buss, DM, Schmitt, DP. Sexual strategies theory: An evolutionary perspective on human mating. Psychol Rev 1993; 100: 204–232. 33. Gangestad, SW, Simpson, JA. The evolution of human mating: Trade-offs and strategic pluralism. Behav Brain Sci 2000; 23: 675–687. 34. Greiling, H, Buss, DM. Women’s sexual strategies: The hidden dimension of extrapair mating. Pers Individ Dif 2000; 28: 929–963. 35. Buss, DM. The evolution of desire: Strategies of human mating. Basic Books: New York, 2003. 36. Buss, DM, Shackelford, TK. From vigilance to violence: Mate retention tactics in married couples. J Pers Soc Psychol 1997; 72: 346–361. 37. Schmitt, DP. Patterns and universals of mate poaching across 53 nations: The effects of sex, culture, and personality on romantically attracting another person. J Pers Soc Psychol 2004; 86: 560–584. 38. Schmitt, DP, Buss, DM. Human mate poaching: Tactics and temptations for infiltrating existing relationships. J Pers Soc Psychol 2001; 80: 894–917. 39. Baker, RR, Bellis, MA. Human sperm competition. Chapman & Hall: London,1995. 40. Shackelford, TK, Pound, N, Goetz, AT, LaMunyon, CW. Female infidelity and sperm competition. In: Buss, DM, ed. The handbook of evolutionary psychology. Wiley: New York 2005, pp. 372–393. 41. Burley, N, Symanski, R. Women without: An evolutionary and cross-cultural perspective on prostitution. In: Symanski, IR, ed. The immoral landscape: Female prostitution in Western societies. Butterworth-Heineman: Toronto, 1981, pp. 239– 274. 42. Baumeister, RF, Mendoza, JP. Cultural variations in the sexual marketplace: gender equality correlates with more sexual activity. J Soc Psychol 2011; 151: 350-60. 43. Symons, D. The evolution of human sexuality. Oxford University Press: Oxford 1979. 44. Carroll, JL, Volk, KD, Hyde, JS. Differences between males and females in motives for engaging in sexual intercourse. Arch Sex Behav 1985; 14: 131–139. 45. Denney, NW, Field, JK, Quadagno, D. Sex differences in sexual needs and desires. Arch Sex Behav 1984;13: 233–245. 46. Klusmann, D. Sexual motivation and the duration of partnership. Arch Sex Behav 2002; 31: 275-287. 47. Giles, KR, McCabe, MP. Conceptualizing women's sexual function: linear vs. circular models of sexual response. J Sex Med 2009; 6: 2761-2771. 48. 48. Carvalheira, AA, Brotto, LA, Leal, I. Women's motivations for sex: exploring the diagnostic and statistical manual, fourth edition, text revision criteria for hypoactive sexual desire and female sexual arousal disorders. J Sex Med 2010; 7: 1454-1463. 49. Hamann, S, Herman, RA, Nolan, CL, Wallen, K. Men and women differ in amygdala response to visual sexual stimuli. Nat Neurosci 2004; 7: 411–416. 51 50. Townsend, J. What women want–what men want: Why the sexes still see love and commitment so 51. Meston, CM, Trapnell, PD, Gorzalka, BB. Ethnic, gender, and length-of-residency influences on sexual knowledge and attitudes. J Sex Res 1998; 35: 176–188. 52. Baumeister, RF, Vohs, KD. Sexual economics: Sex as female resource for social exchange in heterosexual interactions. Pers Soc Psychol Rev 2004; 8: 339–363. 53. Low, BS. Cross-cultural patterns in the training of children: An evolutionary perspective. J Comp Psychol 1989; 103: 313–319. 54. Gangestad, SW, Simpson, JA. Toward an evolutionary history of female sociosexual variation. J Pers 1990; 58: 69–96. 55. Meston, CM, Hamilton, LD, Harte, CB. Sexual motivation in women as a function of age. J Sex Med 2009; 6: 3305-3319. 56. Carvalho, J, Nobre, P. Biopsychosocial determinants of men’s sexual desire: Testing an integrative model. J Sex Med 2011; 8: 754–763. 57. Carvalho, J, Nobre, P. Predictors of men's Sexual Desire: the role of psychological, cognitive-emotional, relational, and medical factors. J Sex Res 2011; 48: 254-262. 58. Althof, S. Erectile dysfunction: Psychotherapy with men and couples. In: Leiblum, S, ed. Principles and 59. Yarhouse, M. Sexual identity development: The influence of valuative frameworks on identity synthesis. Psychotherapy 2001; 38: 331-341. 60. Levine, S. Sexuality in Mid-Life. Plenum Press: New York 1998. 61. Zeuthen, K, Gammelgaard, J. Infantile Sexuality. Scand Psychoanal Rev 2010; 33: 3-12. 62. Bowlby, J. The nature of the child's tie to his mother. Int J Psychoanal 1958; 39: 350373. 63. Stern, DN. The interpersonal world of the infant. Basic Books: New York 1985. 64. Masters, WH, Johnson, VE, Kolodny, RC. Masters and Johnson on Sex and Human Loving. Little, Brown and Company: Boston 1986. 65. Giorni, G, Siccardi, M. Ultrasonographic observation of a female fetus’ sexual behavior in utero. Am J Obstet Gynecol 1996; 175: 753. 66. Johnson, P, Maxwell, D. Prenatal penile length. Ultrasound Obstet Gynecol 2000; 15: 308-310. 67. Galenson, E, Roiphe, H. The emergence of genital awareness during the second year of life. In: Friedman, RC, Richart, RM, Vande Wiele, RL, Stern, LO, eds. Sex differences in behaviour. John Wiley & Sons: New York, 1974, pp.223-231. 68. Simonelli, C, Rossi, R, Tripodi, MF, De Stasio, S, Petruccelli, I. Gender identity disorder and preadolescence: A pilot study. Sexologies 2007; 16: 22-28. 69. Sandnabba, NK, Santtila, P, Wannäs, M, Krook K. Age and gender specific sexual behaviors in children. Child Abuse Negl 2003; 27: 579-605. 70. Green, R. The Sissy Boy Syndrome and the Development of Male Homosexuality. New Haven: Yale University Press, 1987. 71. Saghir, M, Robbins, E. Male and Female Homosexuality. Williams & Wilkins: 52 Baltimore 1973. 72. Herdt, G, McClintock, M. The Magical Age of 10. Arch Sex Behav 1973; 29: 587-606. 73. Gagnon, JH, Rosen, R, Leiblum, S. Cognitive and social science aspects of sexual dysfunction: Sexual scripts in therapy. J Sex Marital Ther 1982; 8: 44- 56. 74. Levine, S, Risen, C, Althof, S. Essay on the diagnosis and nature of paraphilia. J Sex Marital Ther 1990; 16: 89-102. 75. Friedman, R, Downey, J. Sexual Orientation and Psychoanalysis: Sexual Science and Clinical Practice. Columbia University Press: New York, 2002. 76. Larsson, I, Svedin CG. Sexual experiences in childhood: recollections. Arch Sex Behav. 2002; Jun, 31(3): 263-73 77. Levine, S. Sexual Life: A Clinician’s Guide. Plenum Press: New York 1992. 78. Halpern, CT, Udry, JR, Campbell, B, Suchindran, C. Testosterone and pubertal development as predictors of sexual activity: a panel analysis of adolescent males. Psychosom Med 1993; 55: 436-447. 79. Tolman, D, Diamond, L. Desegragating sexuality research: Cultural and biological prespectives on gender and desire. Annu Rev Sex Res 2001; 11: 33-74. 80. Egan, SK, Perry, DG. Gender identity: a multidimensional analysis with implications for psychosocial adjustment. Dev Psychol 2001; 37: 451-463. 81. Yunger, JL, Carver, PR, Perry, DG. Does gender identity influence children's psychological well-being? Dev Psychol 2004; 40: 572-582. 82. Diamond, LM. Female bisexuality from adolescence to adulthood: results from a 10year longitudinal study. Dev Psychol 2008; 44: 5-14. 83. Baumeister, RF. Gender differences in erotic plasticity: the female sex drive as socially flexible and responsive. Psychol Bull 2000; 126: 347–374. 84. Leiblum, S, Sachs, J. Getting the Sex You Want: A Woman’s Guide to Becoming Proud, Passionate and Pleased in Bed. Crown Publishers: New York 2003. 85. Reissing, ED, Andruff, HL, Wentland, JJ. Looking back: the experience of first sexual intercourse and current sexual adjustment in young heterosexual adults. J Sex Res 2012; 49: 27-35. 86. Cate, RM, Long, E, Angera, JJ, Draper, KK. Sexual intercourse and relationship development. Fam Relat 1993; 42: 158-164. 87. Lamont, J, Randazzo, J, Farad, M, Wilkins, A, Daya, D. Psychosexual and social profiles of women with vulvodynia. J Sex Marital Ther 2001; 27: 551-555. 88. McCarthy, B. Sexual secrets, trauma, and dysfunction. J Sex Marital Ther 2002; 28: 353-259. 89. Higgins, JA, Trussell, J, Moore, NB, Davidson, JK. Virginity lost, satisfaction gained? Psychological and psychological sexual satisfaction at heterosexual debut. J Sex Res 2010; 47: 384-394. 90. Haavio-Mannila, E, Kontula, O. Correlates of increased sexual satifaction. Arch Sex Behav 1997; 26: 399-419. 91. Santtila, P, Mokros, A, Hartwig, M, et al. Childhood sexual interactions with other children are associated with lower preferred age of sexual partners including sexual interest in children in adulthood. Psychiatry Res 2010; 175: 154-159. young adults' 53 92. Sprecher, S, Barbee, A, Schwartz, P. Was it good for you too? Gender differences in first sexual intercourse experiences. J Sex Res 1995; 32: 3-15. 93. Carpenter, LM. Gender and the meaning and experience of virginity loss in the contemporary United States. Gender Soc 2002; 16: 345-365. 94. Holland, J, Ramazanoglu, C, Sharpe, S Thomson, R. Deconstructing virginity young people’s accounts of first sex. Sex Relation Ther 2000; 15: 221-232. 95. Tsui, L, Nicoladis, E. Losing it: Similarities and differences in first intercourse experiences of men and women. Can J Hum Sex 2004; 13:95-107. 96. Thompson, S. Putting a big thing into a little hole: teenage girls’ accounts of sexual initiation. J Sex Res 1990; 27: 341-361. 97. Udry, JR, Billy, J. Initiation of coitus in early adolescence. Am Sociol Rev 1987; 52: 841-55. 98. Yang, ML, Fullwood, E, Goldstein, J, Mink, JW. Masturbation in infancy and early childhood presenting as a movement disorder: 12 cases and review of the literature. Pediatrics 2005; 116: 1427-1432. 99. Mallants, C, Casteels, K. Pratical approach to childhood masturbation – a review. Eur J Pediat 2008; 167: 1111-1117. 100. Gagnon, JH, Simon, W. Sexual conduct: The social sources of human sexuality. Aldine: Chicago, 1973. 101. Wiederman, M. The gendered nature of sexual scripts. Family Journal 2005; 13: 496502. 102. Gagnon, JH. The explicit and implicit use of the scripting perspective in sex research. Annu Rev Sex Res 1990; 1: 1-44. 103. Simon, W. Postmodern sexualities. Routledge: New York 1996. 104. Simon, W, Gagnon, JH. Sexual scripts: Permanence and change. Arch Sex Behav 1986; 15: 97-120. 105. Simon, W, Gagnon, JH. A sexual scripts approach. In: Geer, JH, O’Donohue, WT, eds. Theories of human sexuality. Plenum Press: New York 1987, pp. 363-383. 106. Parker, R. Reinventing sexual scripts: sexuality and social change in the Twenty-First Century (The 2008 John H. Gagnon distinguished lecture on sexuality, modernity and change). Sex Res Social Policy 2010; 7: 58-66. 107. Simon, W, Gagnon, JH. Sexual scripts. In: Parker, R, Aggleton, P, eds. Culture, society and sexuality: a reader. University College London Press: London 1999, pp. 29-38. 108. Mahay, J, Laumann, EO, Michaels, S. Race, gender and class in sexual script. In: Laumann, EO, Michael RT, eds. Sex, Love and Health in America. University of Chicago Press: Chicago 2001, pp. 197-238. 109. Gagnon, JH. Script and the coordination of sexual conduct (1974). In: Gagnon, J. An Interpretation of Desire. University of Chicago Press: Chicago, 2004, pp. 59-87. 110. Laumann, EO, Gagnon, J. A sociological perspective on sexual action. In: Parker, RG, Gagnon, JH, eds. Conceiving Sexuality. Routledge: New York, 1995, pp. 183214. 111. Laumann, E, Gagnon, J, Michael, RT, Michaels, S. The Social Organization of 54 Sexuality. University of Chicago Press: Chicago 1994. 112. Ortiz-Torres, B, Williams, SP, Ehrhardt, AA. Urban women’s gender scripts: Implications for HIV prevention. Culture, Health & Sexuality 2003; 5: 1–17. 113. Seal, DW, Ehrhardt, AA. Masculinity and urban men: perceived scripts for courtship, romantic, and sexual interactions with women. Culture, Health & Sexuality 2003; 5: 295-319. 114. McCormick, NB. Sexual script: social and therapeutic implications. J Sex Marital Ther 1987; 2: 3-27. 115. Rosen, R, Leiblum, S. A sexual scripting approach to problems of desire. In: Leiblum, S, Rosen, R, eds. Sexual Desire Disorders. Guilford Press: New York 1988, pp.168191. 116. Weiss, DL. Conclusions: The state of sexual theory. J Sex Res 1998; 35: 100-114. 117. Oliver, M, Hyde, J. Gender differences in sexuality: A meta-analysis. Psychological Bulletin 1993; 114: 29-51. 118. Lippa, RA. On deconstructing and reconstructing masculinity-femininity. J Res Pers 2001; 35: 168-207. 119. Fisher, TD. Parent-child communication about sex and young adolescents’ sexual knowledge and attitudes. Adolescence 1986; 21: 517-527. 120. Purnine, DM, Carey, MP, Jorgenson, RS. Gender differences regarding preferences for specific heterosexual practices. J Sex Marital Ther 1994; 20: 271-287. 121. Sedikides, C, Oliver, MB, Campbell, WK. Perceived benefits and costs of romantic relationships for women and men: Implications for exchange theory. Personal Relationships 1994; 1: 5-21. 122. Taris, TW, Semin, GR. Gender as a moderator of the effect of the love motive and relational context on sexual experience. Arch Sex Behav 1997; 26: 159-180. 123. Eyre, SL, Read, NW, Millstein, SG. Adolescent sexual strategies. J Adolesc Health 1997; 20: 286-293. 124. Greer, AE, Buss, DM. Tactics for promoting sexual encounters. J Sex Res 1994; 31: 185–201. 125. McCormick, NB. Come-ons and put-offs: Unmarried students’ strategies for having and avoiding sexual intercourse. Psychol Women Q 1979; 4: 194–211. 126. Hickman, SE, Muehlenhard, CL. ‘‘By the semi-mystical appearance of a condom’’: How young women and men communicate sexual consent in heterosexual situations. J Sex Res 1999; 36: 258–272. 127. Mitchell, K, Wellings, K. First sexual intercourse: Anticipation and communication. Interviews with young people, J Adolesc 1998; 21: 717–726. 128. Gilbert, LA, Walker, SJ, McKinney, S, Snell, JL. Challenging discourse themes reproducing gender in heterosexual dating: An analog study. Sex Roles 1999; 41: 753–774. 129. Morgan, EM, Zurbriggen, EL. Wanting sex and wanting to wait: Young adults’ accounts of sexual messages from first significant dating partners. Feminism & Psychology 2007; 17: 515–541. 55 130. Kim, JL, Sorsoli, L, Collins, K, Zylbergold, BA, Schooler, D, Tolam, DL. From sex to sexuality: Exposing the heterosexual script on primetime network television. J Sex Res 2007; 44: 145–157. 131. Grauerholz, E, Serpe, RT. Initiation and response: The dynamics of sexual desire. Sex Roles 1985; 12: 1041–1059. 132. Seal, DW, Smith, M, Coley, B, Perry, J, Gamez, M. Urban heterosexual couples’ sexual scripts for three shared sexual experiences. Sex Roles 2008; 58: 626–638. 133. Vannier, SA, O’Sullivan, LF, Communicating interest in sex: verbal and nonverbal initiation of sexual activity in young adults’ romantic dating relationships. Arch Sex Behav 2011; 40: 961-969. 134. Gilfoyle, J, Wilson, J, Own B. Sex, organs and audiotape: A discourse analytic approach to talking about heterosexual sex and relationships. Fem Psychol 1992; 2: 209-230. 135. Grace, V, Potts, A, Gavey, N, Vares, T. The Discursive Condition of Viagra. Sexualities 2006; 9: 295-314. 136. Potts, A, Grace, VM, Vares, T, Gavey, N. 'Sex for life'? Men's counter-stories on 'erectile dysfunction', male sexuality and ageing. Sociol Health Illn 2006; 28: 306-329. 137. Masters, WH, Johnson, VE. Human sexual response. Little Brown: Boston 1966. 138. Masters, WH, Johnson, VE. Human Sexual Inadequacy. Little Brown: Boston 1970. 139. Rosen, R, Beck, J. Patterns of sexual arousal: psychophysiological processes and clinical applications. Guilford Press: New York 1998. 140. Kaplan, HS. The New Sex Therapy. Bruner Mazel: New York 1974. 141. DeRogatis, LR, Clayton, AH, Rosen, RC, Sand, M, Pyke, RE. Should sexual desire and arousal disorders in women be merged? Arch Sex Behav 2011; 40: 217-219. 142. Brotto, LA, Graham, CA, Binik, YM, Segraves, TR, Zucker, KJ. Should Sexual Desire and Arousal Disorders in Women Be Merged? A Response to DeRogatis, Clayton, Rosen, Sand, and Pyke (2010). Arch Sex Behav 2010; 40: 221-225. 143. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition, Text Revision. American Psychiatric Association, Washington DC, 1980. 144. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision. American Psychiatric Association: Washington DC, 2000. 145. Bean, JL. Expressions of female sexuality. J Sex Marital Ther 2002; 28 (Suppl.1): 29–38. 146. Rosen, R, Barsky, JL. Normal sexual response in women. Obstet Gynecol Clin North Am 2006; 33: 515-526. 147. Hayes, RD. Circular and linear modeling of female sexual desire and arousal. J Sex Res 2011; 48: 130-141. 148. Whipple, B, Brash-McGreer, KB. Management of female sexual dysfunction. In: Sipski, ML, Alexander, CJ, eds. Sexual function in people with disability and chronic illness. A health professional’s guide. Aspen Publishers: Gaithersburg 1997, pp. 509– 534. 56 149. Basson, R. Women’s sexual dysfunction: revised and expanded definitions. CMAJ 2005; 172: 1327-1333. 150. Dennerstein, L, Lehert, P. Modeling mid-aged women’s sexual functioning: a prospective, population-based study. J Sex Marital Ther 2004; 30: 173–183. 151. Basson, R, Wierman, ME, van Lankveld, J, Brotto, L. Summary of the Recommendations on Sexual Dysfunction in Women. J Sex Med 2010; 7: 314-326. 152. Bancroft, J. Sexual desire and the brain. J Sex Marital Ther 1989; 3: 11–27. 153. Andersen, B, Cyranowski, J. Women’s sexuality: Behaviors, responses and individual differences. J Consult Clin Psychol 1995; 63: 891-906. 154. Wylie, K, Mimoun, S. Sexual response models in women- Maturitas 2009; 63: 112115. 155. Brotto, LA, Heiman, JR, Tolman, DL. Narratives of desire in mid-age women with and without arousal difficulties. J Sex Res 2009; 46: 387–398. 156. Graham, CA. The DSM diagnostic criteria for female orgasmic disorder. Arch Sex Behav 2010; 39: 256-70. 157. Nobre, PJ, Pinto-Gouveia, J, Gomes FA. Prevalence and comorbidity of sexual dysfunctionsin a Portuguese clinical sample. J Sex Marital Ther 2006; 32: 173–182. 158. Rosen, R, Brown, C, Heiman, J, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of sexual function. J Sex Marital Ther 2000; 26: 191–208. 159. Ter Kuile, MK, Brauer, M, Laan, E. The Female Sexual Function Index (FSFI) and the Female Sexual Distress Scale (FSDS): psychometric properties within a Dutch population. J Sex Marital Ther 2006; 32: 289–304. 160. Graham, CA, Sanders, SA, Milhausen, RR, McBride, KR. Turning on and turning off: A focus group study of the factors that affect women’s sexual arousal. Arch Sex Behav 2004; 33: 527–538. 161. Laan, E, Everaerd, W, van Bellen, G, Hanewald, G. Women’s sexual and emotional responses to male- and female produced erotica. Arch Sex Behav 1994; 23: 153– 169. 162. Chivers, ML, Bailey, JM. A sex difference in features that elicit genital response. Biol Psychol 2005; 70: 115–120. 163. Basson, R. Are our definitions of women’s desire, arousal, and sexual pain disorders too broad and our definition of orgasmic disorder too narrow? J Sex Marital Ther 2002a; 28: 289–300. 164. Both, S, Everaerd, W, Laan, E. Desire emerges from excitement: a psychophysiological perspective on sexual motivation. In: Janssen, E, ed. The Psychophysiology of Sex. Indiana University Press, Bloomington 2007, pp. 327–339. 165. Spiering, M, Everaerd, W, Karsdorp, P, Both, S, Brauer, M. Nonconscious processing of sexual information: a generalization to women. J. Sex Res 2006; 43: 268–281. 166. Garde, K, Lunde, I. Female sexual behaviour. The study in a random sample of 40years-old women. Maturitas 1980; 2: 225-40. 167. Whalen, R. Sexual motivation. Psychol Rev 1966; 73: 151–163. 168. Both, S, Laan, E, Schultz, WW. Disorders in sexual desire and sexual arousal in 57 women, a 2010 state of the art. J Psychosom Obstet Gynaecol 2010; 31: 207-18. 169. Laan, E, Both, S. Sexual desire and arousal disorders in women. Adv Psychosom Med 2011; 31:16-34. 170. Brotto, LA. The DSM diagnostic criteria for Hypoactive Sexual Desire Disorder in women. Arch Sex Behav 2010; 39: 221–239. 171. Graham, CA. The DSM diagnostic criteria for Female Sexual Arousal Disorder. Arch. Sex Behav 2010; 39: 240–255. 172. Sachs, BD. A contextual definition of male sexual arousal. Horm Behav 2007; 51: 569–578. 173. Bancroft, J. Sexual arousal. In: Polk, T, Seifert, C, eds. Encyclopedia of cognitive science. Nature Publishing Group: London, 2002, pp.1165–1168. 174. Ferretti, A, Caulo, M, Del Gratta, C, et al. Dynamics of male sexual arousal: Distinct components of brain activation revealed by fMRI. Neuroimage 2005; 26: 1086–1096. 175. Delizonna, LL, Wincze, JP, Litz, BT, Brown, TA, Barlow, DH. A comparison of subjective and physiological measures of mechanically produced and erotically produced erections (or, is an erection an erection?). J Sex Marital Ther 2001; 27: 21– 31. 176. Rosen, R, Diamond, LE, Earle, DC, Shadiack, AM, Molinoff, PB. Evaluation of the safety, pharmacokinetics and pharmacodynamic effects of subcutaneously administered PT-141, a melanocortin receptor agonist, in healthy male subjects and in patients with an inadequate response to Viagra. Int J Impot Res 2004; 16: 135–42. 177. Miner, M, Seftel, A. Centrally acting mechanisms for the treatment of male sexual dysfunction. Urol Clin North Am 2007; 34: 483–496. 178. Janssen, E, McBride, KR, Yarber, W, Hill, BJ, Butler, SM. Factors that Influence Sexual Arousal in Men: A Focus Group Study. Arch Sex Behav 2008; 37: 252–265. 179. Carpenter, D, Janssen, E, Graham, C, Vorst, H, Wicherts, J. Women’s scores on the Sexual Inhibition/Sexual Excitation Scales (SIS/SES): Gender similarities and differences. J Sex Res 2008; 45: 36-48. 180. Sand, M, Fisher, WA. Women’s endorsement of models of female sexual response: The nurses sexuality study. J Sex Med 2007; 4: 708–719. 181. Meana, M. Elucidating women’s (hetero) sexual desire: Definitional challenges and content expansion. J Sex Res 2010; 47:104–122. 182. Balon, R. The DSM criteria of sexual dysfunction: Need for a change. J Sex Marital Ther 2008; 34: 186–197. 183. Basson, R. Human sex response cycles. J Sex Marital Ther 2001; 27: 33-43. 184. Sand, M, Giraldi, A, Kristensen, E. Men’s endorsement of models of sexual response and motivation for sexual activity. J Sex Med 2010; 7 (Suppl.4): 151-182. 185. Levine, S. Demystifying love. Routledge: New York 2008. 186. Fisher, HE. Lust, attraction, and attachment in mammalian reproduction. Hum Nat 1998; 9: 23–52. 187. Fisher, HE, Aron, A, Mashek, D, Li, H, Brown, LL. Defining the brain systems of lust, romantic attraction and attachment. Arch Sex Behav 2002; 31: 413-419. 58 188. Toates, F. An integrative theoretical framework for understanding sexual motivation, arousal, and behaviour. J Sex Res 2009; 46: 168-193. 189. De, Jong DC. The role of attention in sexual arousal: implications for treatment of sexual dysfunction. J Sex Res 2009; 46: 237-248. 190. Sanders, SA, Graham, CA, Milhausen, RR. Predicting sexual problems in women: the relevance of sexual excitation and sexual inhibition. Arch Sex Behav 2008; 37: 241-251. 191. Janssen, E, Everaerd, W, Spiering, M, Janssen, J. Automatic process and the appraisal of sexual stimuli: toward an information processing model of sexual arousal. J Sex Res 2000; 37: 8-23. 192. Bancroft, J, Janssen, E. The dual control model of male sexual response: a theoretical approach to centrally-mediated erectile dysfunction. Neurosci Biobehav Rev 2000; 24: 571–579. 193. Bancroft, J. Central inhibition of sexual response in the male: a theoretical perspective. Neurosci Biobehav Rev 1999; 23: 763-784. 194. Janssen, E, Vorst, H, Finn, P, Bancroft, J. The Sexual Inhibition (SIS) and Sexual Excitation (SES) Scales: II. Predicting psychophysiological response pattens. J Sex Res 2002; 39:127-132. 195. Carpenter, D, Janssen, E, Graham, C, Vorst, H, & Wicherts, J. Gender similarities in Dual Control Model processes: A short version of the Sexual Inhibition and Excitation Scales (SIS/SES-Short Form) 2006. Poster presented at the 32nd annual meeting of the International Academy of Sex Research (IASR), Amsterdam, The Netherlands, July. 196. Janssen, E, Bancroft, J. The dual-control model: the role of sexual inhibition and excitation in sexual arousal and behaviour. In: Janssen, E, eds. The psychophysiology of sex.: Indiana University Press: Bloomington 2007, pp. 197– 222. 197. Graham, CA, Sanders, SA, Milhausen, RR. The sexual excitation/sexual inhibition inventory for women: psychometric properties. Arc Sex Beahv 2006; 35: 397-409 198. Perelman, M. The sexual Tipping Point: a mind/body model for sexual medicine. J Sex Med 2009; 6: 629-632. 199. Perelman, M. The Sexual Tipping Point: a model to conceptualize etiology, diagnosis & combination treatment of female & male sexual dysfunction. J Sex Med 2006; 3 (Suppl.1): 52. 200. Tiefer, L. Historical, scientific, clinical and feminist criticisms of ‘the human sexual response cycle’ model. Annu Rev Sex Res 1991; 2: 1–23. 201. Leiblum, SR. Definitions and classification of female sexual disorders. Int J Impot Res 1998; 10: 104–106. 202. Baber, KM, Murray, CI. A postmodern feminist approach to teaching human sexuality. Fam Relat 2001; 50: 23–33. 203. Basson, R, Berman, J, Burnett, AL, Derogatis, L, Ferguson, D, Fourcroy J. Report of the international consensus development conference on female sexual dysfunctions: Definitions and classifications. J Urol 2000; 163: 888-93. 204. Metz, M, McCarthy, B. The Good-Enough Sex model for couple satisfaction. Sex Relation Therapy 2007; 22: 351–362. 59 205. McCarthy B, Metz M. The “Good-Enough Sex” model: a case illustration, Sex and Relationship Therapy 2008; 23: 227–234. 206. Metz, M, McCarthy, B. Enduring Desire: Your Guide to Lifelong Intimacy. Routledge: New York 2010. 207. Rutter, M. The interplay of nature, nurture and developmental influences: The challenge ahead for mental health. Arch Gen Psychiatry 2002; 59: 996-1000. 208. Luthar, S. The concept of resilience. Child Development 2000; 71: 534-562. 209. McCabe, M. Childhood, adolescent and current psychological factors associated with sexual dysfunction. J Sex Marital Ther 1994; 9: 267-276. 210. Wylie, KR, Eardley, I. Penile size and the 'small penis syndrome. BJU Int 2007; 99:1449-1455. 211. Ghanem, H, Glina, S, Assalian, P, Buvat, J, Management of Men Complaining of a Small Penis Despite an Actually Normal Size. J Sex Med 2012 Article first published online: 18 APR 2012 DOI: 10.1111/j.1743-6109.2012.02725.x 212. Goins, LB, Markey, CN, Gillen, MM. Understanding Men's Body Image in the Context of Their Romantic Relationships. Am J Mens Health 2012; 6: 240-248. 213. Woertman, L, van den Brink, F. Body image and female sexual functioning and behavior: a review. J Sex Res 2012; 49: 184-211. 214. Pujols, Y, Seal, BN, Meston, CM. The association between sexual satisfaction and body image in women 2010; Feb;7(2 Pt 2):905-16. 215. Seal, BN, Meston, C. The impact of body awareness on sexual arousal in women with sexual dysfunction. J Sex Med 2007; 4: 990-1000. 216. Lowenstein, L, Gamble, T, Sanses TV, et al. Sexual function is related to body image perception in women with pelvic organ prolapse. J Sex Med. 2009; 6: 2286-2291. 217. Ussher, JM, Perz, J, Gilbert, E. Changes to Sexual Well-Being and Intimacy After Breast Cancer. Cancer Nurs 2012 Jan 4. 218. Gilbert, E, Ussher, JM, Perz, J. Sexuality after breast cancer: a review. Maturitas 2010; 66: 397-407. 219. Rossen, P, Pedersen, AF, Zachariae, R, von der Maase, H. Sexuality and body image in long-term survivors of testicular cancer. Eur J Cancer 2012; 48: 571-578. 220. Heiman, J, Rowland, D. Affective and physiological sexual response patterns: The effects of instructions on sexually functional and dysfunctional men. J Psychsom Res 1983; 27: 105-116. 221. Cranston-Cuebas, M, Barlow, D. Cognitive and affective contributions to sexual functioning. Annu Rev Sex Res 1990; 1: 119-161. 222. Beggs, VE, Calhoun, KS, Wolchik, SA. Sexual anxiety and female sexual arousal: A comparison of arousal during sexual anxiety stimuli and sexual pleasure stimuli. Arch Sex Behav 1987; 16: 311-319. 223. Meston, C, Heiman, J. Ephedrine activated physiological sexual arousal in women. Arch Gen Psychiatry 1998; 55: 652-656. 224. Meston, C. Sympathetic nervous system activity and female sexual arousal. Am J Cardiol 2000; 86: 30-34. 60 225. Van Minnen, A, Kampman, M. The interaction between anxiety and sexual functioning: a controlled study of sexual functioning in women with anxiety disorders. Sex Relation Ther 2000; 15: 47-57. 226. Ferguson, J. The effects of antidepressants on sexual functioning in depressed patients: A review. J Clin Psychiatry 2001; 62 (Suppl.3): 22-34. 227. Lykins, A, Janssen, E, Graham, C. The relationship between negative mood and sexuality in heterosexual college women and men. J Sex Med 2006; 43: 136-143. 228. Assalian, P. Erectile dysfunction and depression. J Sex Reprod Med 2003; 3 (Suppl.A): S6-S8. 229. Frolich, PF, Meston, CM. Sexual functioning and self-reported depressive symtpoms among college women. J Sex Res 2002; 39: 321-325. 230. Quinta Gomes, AL, Nobre, P. Personality traits and psychopathology on male sexual dysfunction: An empirical study. J Sex Med 2011; 8: 461–469. 231. Seidman, S, Roose, SP, Menza, MA, Shabsigh, R, Rosen, R. Treatment of erectile dysfunction in men with depressive symptoms. Resuls of a placebo-controlled trial with sildenafil citrate. Am J Psychiatry 2001; 158: 1623-1630. 232. Perelman, M, Rowland, D. Retarded ejaculation. World J Urol 2006; 24: 645-652. 233. Assalian, P. Joint Conference of the American Association of Sex Educators, Counsellors and Therapists and the Society for the Scientific Study of Sex. Boston, Massachusetts, 1984. 234. Michetti, P, Rossi, R, Bonanno, D, Tiesi, I, Simonelli, C. Male sexuality and regulation of emotions: A study on the association between alexithymia and erectile dysfunction (ED). Int J Impot Res 2006; 18: 1170-1174. 235. Michetti, PM, Rossi, R, Bonanno, D, De Dominicis, C, Iori, F, Simonelli, C. Dysregulation of emotions and premature ejaculation (PE): alexithymia in 100 outpatients. J Sex Med 2007; 4:1462-1467. 236. Simonelli, C, Bonanno, D, Michetti, P, Rossi, R. Premature ejaculation and dysregulation of emotions: Research and clinical implications. Sexologies 2008; 17: 18-23. 237. Rowland, D, Cooper, S. Practical tips for sexual counseling and psychotherapy in premature ejaculation. J Sex Med 2011; 8 (Suppl.4): 342–352. 238. Barlow, DH. Causes of sexual dysfunction: The role of anxiety and cognitive interference. J Consult Clin Psychol 1986; 54: 140–148. 239. Barlow, DH. Anxiety and its disorders (2nd edition). The Guilford Press: New York, 2002. 240. Wiegel, M, Scepkowski, LA, Barlow, DH. Cognitive-affective processes in sexual arousal and sexual dysfunction. In: Janssen, E, ed. The psychophysiology of sex. Indiana University Press: Bloomington 2007, pp. 143–165. 241. Purdon, C, Watson, C. Non-erotic thoughts and sexual functioning. Arch Sex Behav 2011; 40: 891-902. 242. Purdon, C, Holdaway, L. Non-erotic thoughts: Content and relation to sexual functioning and sexual satisfaction. J Sex Res 2006; 43: 154–162. 243. Nelson, A, Purdon, C. Non-erotic thoughts, attentional focus, and sexual problems in 61 a community sample. Arch Sex Behav 2011; 40: 395–406. 244. Althof, S. Treatment of Rapid Ejaculation: Psychotherapy, Pharmacotherapy, and Combined Therapy. In: Leiblum, S, ed. Principles and Practice of Sex Therapy (4th Edition). Guilford Press: New York, 2007, pp. 212-240. 245. Althof, S. The patient with erectile dysfunction: psychological issues. Nurse Pract 2000; 25 (Suppl.3): S11-S13. 246. Perelman, M. A new combination treatment for premature ejaculation. A sex therapist’s perspective. J Sex Med 2006; 3: 1004-1012. 247. Sharlip, I, Shumaker, B, Hakim, LS, Goldfischer, E, Natanegara, F, Wong, D. Tadalafil is efficacious and well tolerated in the treatment of erectile dysfunction (ED) in men over 65 years of age: Results from multiple observations in men with ED in national tadalafil study in the United States. J Sex Med 2008; 5: 716-725. 248. Phelps, JS, Jain, A, Monga, M. The PsychoedPlusMed approach to erectile dysfunction treatment: the impact of combining a psychoeducational intervention with sildenafil. J Sex Marital Ther 2004; 30: 305-314. 249. Nobre, PJ, Pinto-Gouveia, J. Cognitions, Emotions, and Sexual Response: Analysis of the Relationship among Automatic Thoughts, Emotional Responses, and Sexual Arousal. Arch Sex Behav 2008; 37: 652–661. 250. Carvalho, J, Nobre, P. Predictors of women’s sexual desire: the role of psychopathology, cognitive-emotional determinants, relationship dimensions, and medical factors. J Sex Med 2010; 7: 928–937. 251. Talmadge, L, Talmadge, W. Relational sexuality: An understanding of low sexual desire. J Sex Marital Ther 1986;12: 3-21. 252. Schnarch, D. Desire problems: A systemic perspective. In: Leiblum, S, Rosen, R, eds. Principles and Practices of Sex Therapy, 3rd Edition. Guilford Press: New York 2000, pp. 17-56. 253. Schnarch D. Intimacy and Desire. Beaufort Books: New York 2009. 254. McCabe, MP, Cobain, M. The impact of individual and relationship factors on sexual dysfunction among males and females. J Sex Marital Ther 1998; 13: 131-143. 255. Hurlbert, D, Fertel, E, Singh, D, Fernandez, F, Menendez, DA, Salgado, C. The role of sexual functioning in the sexual desire adjustment and psychosocial adaptation of women with hypoactive sexual desire. Can J Hum Sex 2005; 14: 15-30. 256. Leiblum, S, Koochaki, P, Rodenberg, C, Rosen, R. Prevalence of low sexual desire and sexual activity levels among population of menopausal women. NAMS Chicago, Illinois 2002. 257. Kelly, M, Strassberg, D, Turner, C. Behavioral assessment of couples’ communication in female orgasmic disorder. J Sex Marital Ther 2006; 32: 81-95. 258. Oberg, K, Fugel-Meyer, K. Swedish women’s distressing sexual dysfunctions: Some concomitant conditions and life satisfaction. J Sex Marital Ther 2005; 2: 169-180. 259. Atwood, J, Klucinec, E, Neaver, E. A combined-constructionist therapeutic approach to couples experiencing erectile dysfunction: Part I. Contemp Fam Ther 2006; 28: 393-402. 260. Rosen, R, Althof, S. Impact of premature ejaculation: The psychological quality of life and sexual relationship consequences. J Sex Med 2008; 5: 1296-1307. 62 261. Chevret-Measson, M, Jaudinot, E, Sullivan, K, Marrel, A, De Gendre, AS. Impact of erectile dysfunction (ED) on sexual life of female partners: assessment with the Index of Sexual Life (ISL) questionnaire. J Sex Marital Ther 2004; 30: 157-172. 262. Fisher, W, Rosen, R, Eardley, I, Sand, M, Goldstein, I. Sexual experience of female partners of men with erectile dysfunction: The female experience of men’s attitudes to life events and sexuality (FEMALES) study. J Sex Med 2005; 2: 675-684. 263. Dean, J, Rubio-Aurioles, E, McCabe, M, et al. Integrating partners into erectile dysfunction treatment: improving the sexual experience for the couple. Int J Clin Pract 2008; 62: 127-133. 264. Riley, A. When treating erectile dysfunction do not forget the partner. Int J Clin Pract 2008; 62: 1-9. 265. Smith, KB, Pukall, CF, Tripp, DA, Nickel, JC. Sexual and relationship functioning in men with chronic prostatitis/chronic pelvic pain syndrome and their partners. Arch Sex Behav 2007; 36: 301-311. 266. Wylie, K. Optimising clinical interventions for sexual difficulties within a relationship. J Mens Health Gend 2006; 4: 350-355. 267. Besharat, M. Management strategies of sexual dysfunctions. J Contemp Psychother 2001; 31: 161-180. 268. Stravynski, A, Gaudettem, G, Lesage, A, et al. The treatment of sexually dysfunctional women without partners: A controlled study of three behavioral group approaches. Clin Psychol Psychother 2007; 14: 211-220. 269. Hawton, K, Catalan, J, Fagg, J. Low sexual desire: Sex therapy results and prognostic factors. Behav Res Ther 1991; 29: 217-224. 270. Sand, M, Fisher, W, Rosen, R, Heiman, J, Eardley, I. Erectile dysfunction and constructs of masculinity and quality of life in the multinational Men’s Attitudes to Life Events and Sexuality (MALES) study. J Sex Med 2008; 5: 583-594. 271. Leiblum, S. After sildenafil: Bridging the gap between pharmacological treatment and satisfying sexual relationships. J Clin Psychiatry 2002; 63: 17-22. 272. Althof, S, Leiblum, S, Chevret, M, et al. Psychological and Interpersonal Dimensions of Sexual Function and Dysfunction. In: Lue, T, Basson, R, Rosen, R, Giuliano, F, Khoury, S, Montorsi, F, eds. Sexual Medicine: Sexual Dysfunctions in Men and Women. Health Publications: Paris, 2004; pp. 73-115. 273. Taylor, A, Gosney, MA. Sexuality in older age: Essential considerations for healthcare professionals. Age Ageing 2011; 40: 538-543. 274. Wylie, K, Kenney, G. Sexual dysfunction and the ageing male. Maturitas 2010; 65: 23-27. 275. Hinchliff, S, Gott, M, Ingleton, C. Sex, menopause and social context: A qualitative study with heterosexual women. J Health Psychol 2010; 15: 724-733. 276. Galinsky, AM. Sexual touching and difficulties with sexual arousal and orgasm among U.S. older adults, Arch Sex Behav 2011; 8: 1-16. 277. Karraker, A, DeLamater, J, Schwartz, CR. Sexual frequency decline from midlife to later life. J Gerontol B Psychol Sci Soc Sci 2011; 66: 502-512. 278. Hyde, Z, Flicker, L, Hankey, GJ, et al. Prevalence of sexual activity and associated factors in men aged 75 to 95 years. Ann Intern Med 2010; 153: 693-702. 63 279. Katz-Bearnot, S. Menopause, depression, and loss of sexual desire: A psychodynamic contribution. J Am Acad Psychoanal Dyn Psychiatry 2010; 38: 99116. 280. Nappi, RE, Lachowsky, M. Menopause and sexuality: Prevalence of symptoms and impact on quality of life. Maturitas 2009; 63: 138-141. 281. Woloski-Wruble, AC, Oliel, Y, Leefsma, M, Hochner-Celnikier, D. Sexual activities, sexual and life satisfaction, and successful aging in women. J Sex Med 2010; 7: 2401-2410. 282. McFarland, MJ, Uecker, JE, Regnerus, MD. The role of religion in shaping sexual frequency and satisfaction: evidence from married and unmarried older adults. J Sex Res 2011; 48: 297-308. 283. Thompson, WK, Charo, L, Vahia, IV, Depp, C, Allison, M, Jeste, DV. Association between higher levels of sexual function, activity, and satisfaction and self-rated successful aging in older postmenopausal women. A Am Geriatr Soc 2011; 59: 15031508. 284. Valadares, ALR, Pinto-Neto, AM, de Souza, MH, Osis, MJD, da Costa Paiva, LHS. The prevalence of the components of low sexual function and associated factors in middle-aged women. J Sex Med 2011; 8: 2851-2858. 285. Kleinplatz, PJ. The profession of sex therapy, Systemic Sex Therapy. Routledge: New York 2008. 286. Moreira, ED, Glasser, DB, Nicolosi, A, Duarte, FG, Gingell, C. Sexual problems and help-seeking behaviour in the United Kingdom and continental Europe. Br J Urol 2008; 101: 1005-1011. 287. Bancroft, J. Sex and aging. N Eng J Med 2007; 357: 820-821 288. Gott, M, Hinchliff, S. How important is sex in later life? The views of older people. Soc Sci Med 2003; 58: 1617-1628. 289. Baldwin, K, Ginsberg, P, Harkaway, RC. Under-reporting of erectile dysfunction among men with unrelated urologic conditions. Int J Impot Res 2003; 15: 87-89. 290. Kaas, MJ. Geriatric sexuality breakdown syndrome. Int J Aging Hum Dev 1981; 13: 71-77. 291. Kinsey, AC, Pomeroy, WB, Martin, CE. Sexual behavior in the human male. Sanders: Philadelphia 1948. 292. Kinsey, A, Pomeroy, W, Martin, C, Gebhard, P. Sexual Behavior in the Human Female. Saunders: Philadelphia 1953. 293. Eriksen, BC. A randomized, open, parallel group study of preventive effect of an estradiol preleasing ring (Estring) on recurrent urinary tract infections in postmenopausal women. Am J Obstet Gynecol 1999; 180: 1072-1079. 294. Abramson PR, Pinkerton SD, 1995, Sexual Nature/Sexual Culture. University of Chicago Press, Chicago. 295. Binik, YM, Meana, M. The future of sex therapy: specialization or marginalization? Arch Sex Behav 2009; 38: 1016-1027. 296. Hernandez Serrano R, Pacheco Palha A, Azim SA, Simonelli C, Navarro Cremades F, Parra A. Advances in Diagnosis and Classification of Sexual Disorders. In: Salloum IM, Mezzich JE, eds. Psychiatric Diagnosis. Challenges and Prospects. Wiley64 Blackwell: Chichester, 2009, pp 129-134. 297. Gurkan, L, Oommen, O, Hellstrom, WJ. Premature ejaculation: Current and future treatments. Asian J Androl 2008; 10: 102-109. 298. Simonelli, C, Fabrizi, A, Rossi, R, Corica, F, Giami, A. Sexology as a profession in Europe: results from an Italian survey. Sexologies 2006;1: 50-57. 299. Giami, A, Practicing sexology in Europe, Sexologies Eur J Sexol 2006:1-71. 65