Curso de Formação “Doenças Infecciosas Víricas”!
Porto, 4 de Outubro de 2014
Diagnóstico laboratorial
das infecções por HBV e
HCV
José Miguel Azevedo Pereira!
!
Professor Auxiliar, Faculdade de Farmácia, Universidade de
Lisboa (FFUL)!
iMed.ULisboa - Unidade interacção Hospedeiro-Patogeno, FFUL !
Centro de Patogénese Molecular, Unidade dos Retrovírus e
Infecções Associadas, FFUL!
Instituto de Medicina Molecular, FFUL!
!
e-mail: [email protected]
HBV e HCV como graves problemas de saúde pública
❖
500 milhões de indivíduos com hepatite crónica de
origem viral!
❖
Mais de 1,5 milhões morrem anualmente de doença
hepática causada pelo HBV e HCV: cirrose
descompensada e carcinoma hepato-celular
J.M. Azevedo Pereira
FFUL
HBV - várias infecções distintas
❖
Infecção primária - assintomática ou sub-clínica!
❖
Infecção primária - hepatite aguda!
❖
Infecção primária - hepatite fulminante!
❖
Infecção persistente - sub-clínica!
❖
Infecção persistente - hepatite crónica
J.M. Azevedo Pereira
FFUL
Infecção primária
❖
❖
Apresentação clínica:!
❖
Assintomática/sub-clínica: mais frequentemente observada nas
crianças!
❖
Hepatite aguda!
❖
Hepatite fulminante (co-infecções HBV/HCV/HDV)!
Período de incubação: ca. 3 meses
J.M. Azevedo Pereira
FFUL
Infecção persistente
❖
Em 5-10% dos adultos e em ca. 90% das crianças
infectadas pelo HBV, a infecção primária não se resolve
e a replicação viral é mantida para além dos 6 meses
após o início da hepatite !
❖
Conduz a dano hepático prolongado (hepatite crónica)
aumentando a ocorrência de cirrose e carcinoma hepatocelular
J.M. Azevedo Pereira
FFUL
Diagnóstico das hepatites
❖
Clínico!
❖
Laboratorial!
❖
Bioquímico!
❖
Virológico
J.M. Azevedo Pereira
FFUL
Diagnóstico laboratorial - bioquímico
AST
ALT
Necrose hepatocelular
colestase
Bil
FA
GGT
Colestase
Necrose hepatocelular
J.M. Azevedo Pereira
FFUL
Diagnóstico laboratorial - virológico
❖
Detecção de componentes virais: antigénios (Ag) e ácido
nucleico!
❖
Detecção de anticorpos específicos dos Ag virais
J.M. Azevedo Pereira
FFUL
Figure 1
(b)
(a)
preS1
E
E
spherical SVP
S
E
RNA-containing
Nucleocapsid
preS2
E1
E2
apo B
DNA-containing
Nucleocapsid
Hepatitis B virion
S - “surface”; invólucro viral; AgHBs
C “core”; cápside viral, AgHBc e AgHBe
P “polymerase”; polimerase viral
X proteína X; transactivadora
E
filamentous SVP
S-protein or S-domain
of M and L protein
M-protein
Myristoylated
L-protein
AI
E
ApoAI
ApoE
AI
E
HCV Lipoviral particle
ApoB
Current
J.M. Azevedo
Pereira Opinio
FFUL
Ganem et al. 2004
J.M. Azevedo Pereira
FFUL
Polimerase (RT)!
Invólucro!
Cápside!
Proteína X
J.M. Azevedo Pereira
FFUL
AgHBe e AgHBc
ATG
Gene c
5’
ATG
pré-Core
TAG
Core
3’
AgHBe
AgHBc
Presente no soro
Presente na partícula viral e na célula infectada
J.M. Azevedo Pereira
FFUL
HBV-marcadores serológicos
❖
❖
❖
Antigénios!
❖
Anticorpos!
❖
AgHbs!
❖
Anti-HBs!
❖
AgHBe
❖
Anti-HBe!
❖
Anti-HBc
DNA HBV!
cccDNA
Sangue periférico - soro
Hepatócito
J.M. Azevedo Pereira
FFUL
The
new england journal
of
medicine
Antigen or Antibody Level
A Acute Self-Limited HBV Infection
HBV DNA
HBeAg
Anti-HBs
HBsAg
Anti-HBc
Anti-HBe
ALT
0
5
10
15
20
48
2
Weeks since Exposure
4
6
8
>10
Years since Exposure
Antigen or Antibody Level
B Chronic HBV Infection
Hepatite aguda auto-limitada
HBV DNA
HBeAg
HBV-marcadores
serológicos
Anti-HBs
0
5
10
15
Weeks since Exposure
20
48
HBsAg
Anti-HBc
Ganem et al. 2004
Anti-HBe
ALT
2
4
6
8
>10
Years since Exposure
J.M. Azevedo Pereira
FFUL
A
ALT
0
5
10
15
20
48
2
Weeks since Exposure
4
6
8
>10
Years since Exposure
Antigen or Antibody Level
B Chronic HBV Infection
HBV DNA
HBeAg
Anti-HBs
HBsAg
Anti-HBc
Anti-HBe
ALT
0
5
10
15
20
48
Weeks since Exposure
2
4
6
8
>10
Years since Exposure
Figure 4. Patterns of Serologic and Molecular Markers in HBV Infection.
Typical levels of alanine aminotransferase (ALT), HBV DNA, hepatitis B s and e antigens (HBsAg and HBeAg), and antiInfecção
persistente
- hepatite
crónica
HBc,
anti-HBe,
and anti-HBs
antibodies
are shown in acute self-limited HBV infection (Panel A) and in infections that
become chronic (Panel B). The intensity of the responses, as a function of time after infection, is indicated schematically.
HBV DNA may persist for many years after the resolution of acute self-limited infection.42
HBV-marcadores
serológicos
Ganem et al. 2004
sistently abnormal levels of alanine aminotransfer- begin. Furthermore, screening is imperfect — alpha
ase and elevated levels of viral DNA may denote a fetoprotein screening, for example, has an excelpresubgroup of HBeAg-negative carriers who should lent negative predictive value, but its positive
J.M. Azevedo Pereira
FFUL
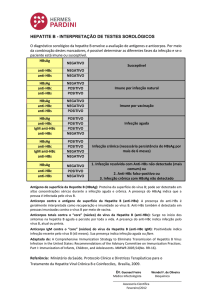
Hepatitis B serologic testing involves measurement of several hepatitis B
virus (HBV)-specific antigens and antibodies. Different serologic “markers”
or combinations of markers are used to identify different phases of HBV
infection and to determine whether a patient has acute or chronic HBV
infection, is immune to HBV as a result of prior infection or vaccination, or
is susceptible to infection.
■
Hepatitis B surface
antigen (HBsAg):
A protein on the surface
of hepatitis B virus; it can
be detected in high levels
in serum during acute or
chronic hepatitis B virus
infection. The presence of
HBsAg indicates that the
person is infectious. The
body normally produces
antibodies to HBsAg as
part of the normal immune
response to infection.
HBsAg is the antigen used
to make hepatitis B vaccin
Interpretação de resultados laboratoriais
MMWR 2005
Tests
Results
Interpretation
HBsAg
anti-HBc
anti-HBs
negative
negative
negative
Susceptible
HBsAg
anti-HBc
anti-HBs
negative
positive
positive
Immune due to natural infection
HBsAg
anti-HBc
anti-HBs
negative
negative
positive
Immune due to hepatitis B vaccination
HBsAg
anti-HBc
IgM anti-HBc
anti-HBs
positive
positive
positive
negative
Acutely infected
HBsAg
anti-HBc
IgM anti-HBc
anti-HBs
positive
positive
negative
negative
Chronically infected
HBsAg
anti-HBc
anti-HBs
negative
positive
negative
Interpretation unclear; four possibilities:
1. Resolved infection (most common)
2. False-positive anti-HBc, thus susceptible
3. “Low level” chronic infection
4. Resolving acute infection
■
■
Hepatitis B surface
antibody (anti-HBs):
The presence of anti-HBs
is generally interpreted as
indicating recovery and
immunity from hepatitis B
virus infection. Anti-HBs
also develops in a person
who has been successfully
vaccinated against
hepatitis B.
Total hepatitis B core
antibody (anti-HBc):
Appears at the onset
of symptoms in acute
hepatitis B and persists
for life. The presence of
anti-HBc indicates previou
J.M. Azevedo Pereira
or ongoingFFUL
infection with
Tests
Results
Interpretation
HBsAg
anti-HBc
anti-HBs
negative
negative
negative
Susceptible
HBsAg
anti-HBc
anti-HBs
negative
positive
positive
Immune due to natural infection
HBsAg
anti-HBc
anti-HBs
negative
negative
positive
Immune due to hepatitis B vaccination
HBsAg
anti-HBc
IgM anti-HBc
anti-HBs
positive
positive
positive
negative
Acutely infected
HBsAg
anti-HBc
IgM anti-HBc
anti-HBs
positive
positive
negative
negative
Chronically infected
HBsAg
anti-HBc
anti-HBs
negative
positive
negative
Interpretation unclear; four possibilities:
1. Resolved infection (most common)
2. False-positive anti-HBc, thus susceptible
3. “Low level” chronic infection
4. Resolving acute infection
HBsAg indicates that the
person is infectious. The
body normally produces
antibodies to HBsAg as
part of the normal immun
response to infection.
HBsAg is the antigen use
to make hepatitis B vacc
■
■
Adapted from: A Comprehensive Immunization Strategy to Eliminate Transmission of Hepatitis B
Virus Infection in the United States: Recommendations of the Advisory Committee on Immunization
Practices. Part I: Immunization of Infants, Children, and Adolescents. MMWR 2005;54(No. RR-16).
■
DEPARTMENT OF HEALTH & HUMAN SERVICES
Centers for Disease Control and Prevention
Dény et al. Path Biol 2010
Division of Viral Hepatitis
Hepatitis B surface
antibody (anti-HBs):
The presence of anti-HBs
is generally interpreted as
indicating recovery and
immunity from hepatitis B
virus infection. Anti-HBs
also develops in a person
who has been successfull
vaccinated against
hepatitis B.
Total hepatitis B core
antibody (anti-HBc):
Appears at the onset
of symptoms in acute
hepatitis B and persists
for life. The presence of
anti-HBc indicates previo
or ongoing infection with
hepatitis B virus in an
undefined time frame.
IgM antibody to hepatitis
core antigen (IgM anti-HB
Positivity indicates recent
infection with hepatitis B
virus (<6 mos). Its presenc
indicates acute infection.
J.M. Azevedo Pereira
FFUL
anti-HBc
anti-HBs
negative
positive
HBsAg
anti-HBc
IgM anti-HBc
anti-HBs
positive
positive
positive
negative
Acutely infected
HBsAg
anti-HBc
IgM anti-HBc
anti-HBs
positive
positive
negative
negative
Chronically infected
HBsAg
anti-HBc
anti-HBs
negative
positive
negative
Interpretation unclear; four possibilities:
1. Resolved infection (most common)
2. False-positive anti-HBc, thus susceptible
3. “Low level” chronic infection
4. Resolving acute infection
an
Th
is
in
im
vi
al
w
va
he
■
Adapted from: A Comprehensive Immunization Strategy to Eliminate Transmission of Hepatitis B
Virus Infection in the United States: Recommendations of the Advisory Committee on Immunization
Practices. Part I: Immunization of Infants, Children, and Adolescents. MMWR 2005;54(No. RR-16).
■
Dény et al. Path Biol 2010DEPARTMENT OF HEALTH & HUMAN SERVICES
J.M. Azevedo Pereira
FFUL
To
an
Ap
of
he
fo
an
or
he
un
Ig
co
Po
in
vi
Antigen or Antibody
IgM anti-HBc
anti-HBs
0
5
HBsAg
anti-HBc
IgM anti-HBc
anti-HBs
10
positive
negative
viru
als
wh
vac
he
HBeAg
Anti-HBs
HBsAg
15
positive
positive
negative
negative
20
Chronically infected
Anti-HBc
Anti-HBe
ALT
■
48
2
4
6
8
>10
Antigen or Antibody Level
Weeks since Exposure
HBsAg
negative
anti-HBc
positive
anti-HBs
negative
B Chronic HBV Infection
HBV DNA
Anti-HBc
AgHBs
Years since
Interpretation unclear;
fourExposure
possibilities:
Ganem et al. 2004
1. Resolved infection (most common)
2. False-positive anti-HBc, thus susceptible
3. “Low level” chronic infection
HBV DNA
AgHBe
4. Resolving acute infection
HBeAg
Adapted from: A Comprehensive Immunization Strategy to Eliminate Transmission of Hepatitis B
Virus Infection in the United States: Recommendations of the Advisory Committee on Immunization
Practices. Part I: Immunization of Infants, Children, and Adolescents. MMWR 2005;54(No. RR-16).
Anti-HBs
HBsAg
Anti-HBc
Anti-HBe
■
ALT
0
5
10
15
20
48
2
4
6
8
>10
Weeks since Exposure
Years since Exposure
ALT
DEPARTMENT OF HEALTH & HUMAN SERVICES
Anti-HBe
Centers for Disease Control and Prevention
Figure 4. Patterns of Serologic and Molecular Markers in HBV Infection.
Division of Viral Hepatitis
Typical levels of alanine aminotransferase (ALT), HBV DNA, hepatitis B s and e antigens (HBsAg and HBeAg), and antiHBc, anti-HBe, and anti-HBs antibodies are shown in acute self-limited HBV infection (Panel A) and in infections that
www.cdc.gov/hepatitis
become chronic (Panel B). The intensity of the responses, as a function of time after infection, is indicated schematically.
HBV DNA may persist for many years after the resolution of acute self-limited infection.42
J.M. Azevedo Pereira
FFUL
To
an
Ap
of
he
for
an
or
he
un
IgM
co
Po
infe
viru
ind
anti-HBs
negative
HBsAg
anti-HBc
anti-HBs
negative
positive
negative
■
Interpretation unclear; four possibilities:
1. Resolved infection (most common)
2. False-positive anti-HBc, thus susceptible
3. “Low level” chronic infection
4. Resolving acute infection
Adapted from: A Comprehensive Immunization Strategy to Eliminate Transmission of Hepatitis B
Virus Infection in the United States: Recommendations of the Advisory Committee on Immunization
Practices. Part I: Immunization of Infants, Children, and Adolescents. MMWR 2005;54(No. RR-16).
■
DEPARTMENT OF HEALTH & HUMAN SERVICES
Centers for Disease Control and Prevention
Division of Viral Hepatitis
www.cdc.gov/hepatitis
Dény et al. Path Biol 2010
J.M. Azevedo Pereira
FFUL
Situações de difícil interpretação
❖
Infecção por mutantes na região pré-core do gene c!
❖
Infecção por mutantes no determinante antigénico “a”
do AgHBs!
❖
Hepatite crónica oculta
J.M. Azevedo Pereira
FFUL
Hepatite por mutantes na região pré-core do gene c
ATG
Gene c
5’
ATG
TAG
pré-Core
TGG
1896
Core
3’
TAG
AgHBe
AgHBc
Não!
mutante
AgHBc
Mutante do !
pré-core
J.M. Azevedo Pereira
FFUL
Hepatite por mutantes
na região “a” do AgHBs
Yim et al. 2008
❖
Substituição Gly/
Arg 145
J.M. Azevedo Pereira
FFUL
Consequências da mutação Gly-Arg 145
❖
Confere resistência aos anticorpos neutralizantes (antiHBs)!
❖
Coexistência de AgHBs e Anti-HBs no soro!
❖
Mutantes têm menor “fitness viral”
J.M. Azevedo Pereira
FFUL
Infecção oculta por HBV (OBI)
1999
❖
Caracterizada por:!
❖
presença de DNA HBV no hepatócito (cccDNA)!
❖
presença ou ausência de DNA HBV soro!
❖
ausência de AgHBs no soro
J.M. Azevedo Pereira
FFUL
Infecção oculta por HBV (OBI)
❖
OBI é ainda caracterizada por:!
❖
Presença de anticorpos anti-HBs e anti-HBc (80% dos
casos)!
❖
Nos restantes 20%, todos os marcadores serológicos
são negativos
J.M. Azevedo Pereira
FFUL
Factores determinantes da OBI
❖
❖
Factores do hospedeiro!
❖
Imunológicos: forte resposta imunológica (linfócitos T-CD4 e T-CD8) que
suprime a replicação do HBV!
❖
Epigenéticos: hipoacetilação das histonas associadas ao cccDNA;
metilação do cccDNA!
Factores virais!
❖
❖
Mutações no AgHBs…!
Coinfecções!
❖
HBV/HCV (proteínas do core do HCV como supressoras da replicação
do HBV)
J.M. Azevedo Pereira
FFUL
Diagnóstico laboratorial da
infecção por HCV
HCV - Epidemiologia
❖
Infecção assintomática em 50-90% dos casos de
infecções agudas por HCV!
❖
Evolução para hepatite crónica em 50-90% dos casos!
❖
130-210 milhões infecções crónicas pelo HCV (3% da
população mundial)!
❖
Seis genótipos (1-6) e vários subtipos!
❖
Transmissão sanguínea, sexual e vertical
J.M. Azevedo Pereira
FFUL
História natural da infecção
LIVER INFECTIONS
Exposure to hepatitis C virus
Mean incubation 6–8 weeks
Acuteinfection
Acute infection
RNA usually detectable by 1–2 weeks
15–40% infection clearance
Chiifti
Chronic infection
Enhanced progression
Disease progression not generally
affected by genotype or viral load
Alcohol
Male
Older age
Diabetes
Infection duration
coinfection
Obesity
H IV /HBV
Insulin resistance
Cirrhosis
Cirrhosis
~20% at 20–30 years after infection
Typically asymptomatic until:
Lever et al.!
2011
Liver failure
2–5% of cirrhotics per year
HBV, hepatitis B virus; HIV, human immunodeficiency virus.
Hepatocellular carcinoma
1–4% of cirrhotics per year
J.M. Azevedo Pereira
FFUL
Diagnóstico laboratorial da infecção por HCV
❖
Pesquisa de anticorpos específicos!
❖
Testes de rastreio!
❖
Testes de confirmação (?)!
❖
Detecção e quantificação do RNA viral (RT-PCR,
bDNA).!
❖
Genotipagem
J.M. Azevedo Pereira
FFUL
Evolução dos marcadores laboratoriais
Infecção aguda auto-limitada
Infecção crónica após infecção aguda
http://depts.washington.edu/hepstudy/hepC/clindx/acute/discussion.html
J.M. Azevedo Pereira
FFUL
HCV
antibody
Reactive
Nonreactive
Not Detected
HCV RNA
Detected
No HCV antibody detected
No current HCV infection
Current HCV infection
STOP*
Additional testing as appropriate†
Link to care
Interpretação dos
resultados laboratoriais
* For persons who might have been exposed to HCV within the past 6 months, testing for HCV RNA or follow-up testing for HCV antibody is recommended. For persons who are
immunocompromised, testing for HCV RNA can be considered.
†
To differentiate past, resolved HCV infection from biologic false positivity for HCV antibody, testing with another HCV antibody assay can be considered. Repeat HCV RNA testing if the person tested
is suspected to have had HCV exposure within the past 6 months or has clinical evidence of HCV disease, or if there is concern regarding the handling or storage of the test specimen.
Recommended Testing Sequence for Identifying
Current Hepatitis C Virus (HCV) Infection
Source: CDC. Testing for HCV infection: An update of guidance for clinicians and laboratorians. MMWR 2013;62(18).
HCV
J.M. Azevedo Pereira
FFUL
Bibliografia
1. Ganem D, Prince AM. Hepatitis B virus infection--natural history and clinical
consequences. N. Engl. J. Med. 2004;350:1118–29.!
2. Dény P, Zoulim F. Hepatitis B virus: from diagnosis to treatment. Pathol. Biol.
(Paris). 2010;58:245–53.!
3. Cacciola I, Pollicino T, Squadrito G, Cerenzia G, Orlando ME, Raimondo G.
Occult hepatitis B virus infection in patients with chronic hepatitis C liver disease.
N Engl J Med. 1999;341:22-6.!
4. Lever C, Nash KL. Hepatitis C. Medicine (Baltimore). 2011;39:550–5.
J.M. Azevedo Pereira
FFUL